Texas Child Protection Law Bench Book
Updated September 2025
Health
Health Care for Texas Children in Foster Care: STAR Health
Introduction
Please see the Checklist Section for the Medical and Mental Health Care for Foster Youth Checklist.
STAR Health is a comprehensive, managed care program operated by one statewide managed care organization designed to better coordinate and improve access to health care for:
• Children in DFPS conservatorship (under age 18);
• Young adults in DFPS Extended Foster Care (age 18 through the month of the person's 22nd birthday);
• Young adults who were previously under DFPS conservatorship and who have returned to foster care through voluntary foster care agreements (age 18 through the month of the person's 21st birthday); and
• Young adults who aged out of foster care at age 18 and who are eligible for Medicaid services (age 18 through 20 years).
Not all children are eligible for the STAR Health program. STAR Health does not cover children who are:
• In state conservatorship who are placed outside of Texas;
• From other states but placed in Texas;
• From other states who are placed in Texas Medicaid-paid facilities, such as children in nursing homes, Intermediate Care Facilities for Individuals with an Intellectual Disability (ICF-IID), or State-Supported Living Centers; or
• In DFPS conservatorship but adjudicated and placed in a Texas Juvenile Justice Department (TJJD) facility. (This population receives healthcare services through TJJD.)
Unless otherwise indicated, children who are ineligible for STAR Health benefits receive Medicaid through fee-for-service Medicaid.
Adoption Assistance/Permanency Care Assistance (AA/PCA)
• Children in Adoption Assistance or Permanency Care Assistance will be enrolled in STAR, STAR Health, or STAR Kids after a transition period. During the transition period they remain enrolled in STAR Health.
• Adoption Assistance/Permanency Care Assistance members who get Supplemental Security Income (SSI), Medicare, or 1915(c) waiver services can choose whether to stay in STAR Health or enroll in STAR Kids.
A. Unique Features of STAR Health
For those children who are covered by STAR Health, STAR Health provides a full range of Medicaid-covered medical, dental, vision, prescription, behavioral health services, in addition to service coordination, information sharing and other program benefits, including:
• A Medical Home for each child (meaning a doctor, or other Primary Care Provider (PCP), or PCP Team to oversee care);
• Immediate enrollment for immediate healthcare benefits;
• Access to health care through a network of providers (doctors, nurses, hospitals, clinics, psychiatrists, therapists, etc.) specifically recruited for their history and expertise in treating children who have been abused or neglected and who are offered ongoing trainings on such issues;
• The Health Passport, which is a web-based, secure health information tool which utilizes claims data to provide information on healthcare services including Texas Health Steps medical checkups, immunizations, lab results, prescriptions, the Family Strengths and Needs Assessments (FSNA), the Texas Child and Adolescent Needs and Strengths (CANS) assessments, Psychotropic Medication Utilization Reviews (PMUR), and service plans to medical consenters, caseworkers, and healthcare providers;
• PMURs to determine if the prescribed medication treatment are within the parameters outlined in the Psychotropic Medication Utilization Parameters for Children and Youth in Texas Public Behavioral Health (7th Edition) (Parameters);[113]
• STAR Health liaisons who work directly with DFPS Well-Being Specialists and DFPS Clinical Coordinators to assist with resolving any barriers to services that children in foster care might encounter;
• STAR Health service Coordinators who work directly with the youth and caregiver to assist with service delivery. This includes annual face-to-face visits and regular telephonic outreach. The STAR Health service coordination is a three-tiered model to administer specialized care management;
• Disease management which provides coordinated healthcare interventions and health education for members with asthma, diabetes, and other chronic or complex conditions, including behavioral health conditions or diseases;
• STAR Health Specialty Court liaisons work with the judiciary and court team to educate on STAR Health benefits to avoid gaps in care and service delays.
• STAR Health transition Coordinators to assist youth with activities to ensure a smooth transition to independence and adulthood, including education about their medical care and referrals to support services, as needed;
• Medical advisory committees to monitor healthcare provider performance; and
• The following are features of all Medicaid managed care programs:
◦ nursing and behavioral health 24/7 helplines for caregivers and caseworkers; and
◦ licensed and degreed managed care organization (MCO) staff and service coordination teams who coordinate physical and behavioral healthcare and access to other non-Medicaid benefits and resources, including for complex cases.
B. Physical Healthcare Benefits Provided by STAR Health
Medicaid-covered physical healthcare benefits include but are not limited to:
• Ambulance services;
• Applied Behavior Analysis services for the treatment of autism for children through 20 years of age;
• Birthing services provided by a physician and Certified Nurse Midwife (CNM) in a licensed birthing center;
• Cancer screening, diagnostic, and treatment services;
• Chiropractic services;
• Community First Choice[114] services, which is a federal program that includes personal assistance services, habilitation, emergency response services, and support consultation;
• Dental services;
• Durable medical equipment and medical supplies;
• Early Childhood Intervention (ECI) services;
• Family planning;
• Hearing exams/hearing aids;
• Home healthcare services, such as private duty nursing, skilled nursing, and personal care services;
• Hospital care, including emergency and inpatient services;
• Lab tests/x-rays;
• Physical, occupational, and speech therapies;
• Podiatry;
• Prenatal care;
• Prescription drugs and biological drugs;
• Preventive care through Texas Health Steps;
• Specialty physician services;
• Telemedicine/telehealth services (applies to certain procedure codes);
• Organs and tissue transplant services; and
• Vision services.
C. Behavioral Health Benefits Provided by STAR Health
Medicaid-covered behavioral health benefits include:
• Outpatient Mental Health Services to include psychotherapy (individual, group, and family), psychiatric diagnostic evaluation with and without medical services, psychological, neurobehavioral and neuropsychological testing, and pharmacological management;
• For members 20 years of age and younger, Mental Health Targeted Case Management to include intensive and routine case management services;
• Mental Health Rehabilitation Services to include crisis intervention services (including mobile crisis services), medication training and support, and skills training and development (can be provided to the child/youth, Legally Authorized Representative [LAR] or primary caregiver);
• Inpatient psychiatric services that include admissions to acute care hospitals and institutions for mental disease (IMDs) (public or private psychiatric facility);[115]
• Substance use disorder services to include assessment, counseling (individual and group), residential treatment, and withdrawal management and Medication-Assisted Treatment (MAT) services;
• Screening, Brief Intervention, and Referral to Treatment (SBIRT) services for persons 10 years of age and older;
• For members 20 years of age and younger, Health and Behavior Assessment and Intervention (HBAI) services;
• Collaborative Care Model (CoCM) services that integrate the services of behavioral healthcare managers (BHCMs) and psychiatric consultants with primary care provider oversight to proactively manage behavioral health conditions as chronic diseases, rather than treating acute symptoms;
• Telemedicine/telehealth services (applies to certain procedure codes);
• Court-ordered services (outpatient and inpatient), if the person is not considered to be incarcerated; and
• In-lieu-of services (ILOSs) and settings offered by the STAR Health MCO that substitute for Medicaid state plan services or settings, as allowed under federal regulations. ILOSs must be a medically appropriate and cost-effective substitute for the covered service or setting under the Medicaid state plan. The Medicaid member must not be required by the MCO to use the ILOS and the MCO is not required to offer it. The following new services were added Medicaid ILOSs as part of the implementation of Senate Bill 1177 (86R): partial hospitalization services, intensive outpatient program services, and Coordinated Specialty Care.
D. Transitioning Foster Care Youth
The Patient Protection and Affordable Care Act (PPACA), commonly called the Affordable Care Act (ACA), requires states to provide Medicaid coverage to youth and young adults under age 26 years who were in foster care and were receiving Medicaid when they aged out of foster care.
The Former Foster Care Children (FFCC) program provides healthcare coverage to youth who aged out of foster care at age 18 years, were receiving Medicaid coverage at the time they aged out, who are a U.S. citizen, and meet all other Medicaid eligibility criteria. This coverage is available through age 25 years under two separate programs, based on age:
• Young adults ages 18 through 20 years are automatically enrolled in the STAR Health program, but can switch to the STAR program, if they prefer; and
• Young adults ages 21 through 25 years must choose a STAR or STAR+PLUS program health plan.
For foster youth who are under the age of 21 years but who are not eligible for the FFCC program because the youth did not receive Medicaid at the time they aged out of care, coverage is provided by the Medicaid for Transitioning Youth (MTFCY) program in STAR Health for youth who:
• Were in DFPS conservatorship on their 18th birthday or older;
• Do not have other health coverage and meet program rules for income;
• Meet program rules for income; and
• Are a US citizen or have a qualified alien status, such as a green card.
It is not necessary for a court to extend jurisdiction beyond age 18 years for this coverage to apply. For more information, see the Extending Foster Care for Transitioning Youth chapter of this Bench Book.
Special Issue: All Medicaid recipients, including youth formerly in foster care, must renew their Medicaid eligibility once every 12 months. To ensure continuous coverage, youth must provide their current mailing address to HHSC. If a youth changes their address without notifying HHSC, and HHSC receives returned mail and cannot locate the youth, the youth's Medicaid benefits will be denied. A youth can report an address change online through www.YourTexasBenefits.com, the Your Texas Benefits mobile app, by calling 2-1-1 (Option 2 after selecting a language), in person at a local Medicaid eligibility office, or by reporting the change in writing by mail or by fax. Youth must also respond to requests for information from HHSC and may need to verify that they are a Texas resident or their immigration status. As of December 10, 2022, youth formerly in foster care can self-attest to their Texas residency at application and redetermination rather than provide documentation (such as a driver's license or a utility bill).
E. Child and Family Assessments
Texas Health Steps: All children entering DFPS conservatorship must receive a comprehensive, preventive healthcare checkup within 30 days of entering DFPS conservatorship known as the “Texas Health Steps” medical checkup. The checkup helps identify the child's unique healthcare needs and helps DFPS make decisions that are in the child's best interest. This checkup is repeated annually or according to the Texas Health Steps periodicity schedule.
Medical Exam Within Three Business Days: Beginning September 1, 2023, a change to the “Three-Day Exam” policy means that not all children will automatically receive a Three-Day Exam. Only qualifying children who enter DFPS conservatorship will receive an initial medical examination from a physician or other healthcare provider authorized by state law to conduct a medical examination by the end of the third business day after the child is removed from the child's home. Tex. Fam. Code § 264.1076. Qualifying circumstances are if the child was removed for physical or sexual abuse, has an obvious physical injury, has a chronic medical condition, is medically complex, or has a diagnosed mental illness. Tex. Fam. Code § 264.1076. Each child is assessed individually for qualification. Exceptions include the youth being in an inpatient hospital setting or requiring urgent medical treatment at the time of removal.
Vaccinations Prohibited During Three-Day Exam: A physician or healthcare provider cannot administer a vaccination at this “Three-Day Exam” without parental consent except for an emergency tetanus vaccination, and only if the physician or other healthcare provider determines that an emergency requires a vaccination. The prohibition of vaccinations does not apply once DFPS is named the child's managing conservator. The restriction on vaccinations applies only to vaccinations (except for tetanus) administered under the medical exam required by Tex. Fam. Code § 264.1076. Thus, the prohibition is limited only to the population receiving the exam and only restricts what can be done during the exam. This restriction is lifted once DFPS is granted conservatorship. Outside of these circumstances, the law neither expands nor restricts a parent's right to withhold consent for immunization either under Tex. Fam. Code § 32.101 or Tex. Health & Safety Code § 161.004. However, see Tex. Fam. Code § 266.002 and Tex. Fam. Code § 266.004 regarding a court's authorization to issue orders related to medical care for children in foster care. See In re Womack, 549 S.W.3d 760 (Tex. App.—Waco 2017) holding that to the extent Tex. Fam. Code § 266.004 and Tex. Fam. Code § 32.101(c) conflict, Tex. Fam. Code § 32.101(c) is more specific and is the controlling statute.
Texas Child and Adolescent Needs and Strengths (CANS) Assessment: Children and youth ages 3 to 17 years must receive a CANS Assessment completed by an in-network STAR Health clinician within 30 days of removal. Prior to conducting the CANS, the CPS caseworker will conduct the FSNA with the family, identify targeted interventions, and work with the family to prioritize goals and tasks.
DFPS uses the results of the CANS to evaluate each child's needs and strengths. This assessment assists in service planning, informs placement decisions, and reduces the number of assessments administered to children in DFPS conservatorship. As of January 1, 2025, DFPS began using an enhanced CANS 3.0 assessment tool.[116]
Family Strength and Needs Assessment (FSNA): DFPS administers the FSNA to assess how the family is functioning and to aid in developing a plan of service for the family. Although the FSNA and CANS will not be attached to court reports, judges may hear DFPS staff providing testimony or information regarding findings or recommendations that come from these assessments.
Special Issue: Many courts prefer to schedule a Status Hearing within a few days of the Adversary Hearing to jump-start services to families. However, this must be balanced with the need for both the STAR Health clinician and the CPS caseworker to have the time to utilize the CANS and FSNA tools with fidelity. The law requires that the CANS be administered within 45 days of removal, and DFPS policy sets the completion date at 30 days. The FSNA is conducted with the family within the first three weeks of removal and is used to inform the CANS. Allowing time for a thorough assessment and coordination of efforts should produce child and family service plans that set a path toward achieving permanency as quickly as possible for the child and family.
Developmental Disability Assessment: DFPS is also required to assess whether a child has a developmental disability as soon as possible after the child is placed in DFPS conservatorship, and if the assessment indicates an intellectual disability, to ensure that a referral for a determination of such is made as soon as possible. Tex. Fam. Code § 264.1075.
F. Medical Consent
Generally, healthcare providers require someone with the legal authority to consent to medical care for a child to provide informed consent for the child before the healthcare provider will initiate care. Texas law requires the court to specifically authorize an individual or DFPS to consent to medical care for each child in DFPS conservatorship. Tex. Fam. Code §§ 153.371-153.377 and Tex. Fam. Code § 266.004(c) provide the legal bases for DFPS' authority to make medical decisions for children and youth in DFPS conservatorship. When the court authorizes DFPS to consent to the child's medical care, the caseworker must designate a medical consenter, a backup medical consenter, and coordinate medical information. It is the responsibility of the medical consenter and backup medical consenter to become knowledgeable of the child's medical condition, known medical history, and medical needs before consenting to medical care or treatment.
1. Informed Consent
Medical consent means making a decision on whether to agree to or not agree to a medical test, treatment, procedure, or a prescription medication. Informed consent means the medical consenter gets complete information about the proposed medical care to provide an understanding of the benefits and risks of the treatment before making a decision. The goal is to make sure that the “medical consenter” makes an informed decision about the child's health care.
Before consenting to any health care, the medical consenter must understand:
• The child's symptoms and medical diagnosis;
• How the treatment will help the condition;
• What happens if the treatment is not applied; and
• The side effects and risks associated with the treatment. See Tex. Fam. Code § 266.004(h); CPS Policy Handbook § 11130.
Special Issue: A person otherwise authorized to consent to the immunization of a child may not consent for the child if the person has actual knowledge that a parent, managing conservator, guardian, or other person who under the law of another state or a court order may consent for the child and has expressly refused to give consent to the immunization, has been told not to consent for the child, or has withdrawn a prior written authorization for the person to consent. Tex. Fam. Code § 32.101(c).
2. Choosing a Medical Consenter
When a judge gives DFPS the authority to consent to medical care for a child in conservatorship, the agency designates up to four primary and/or backup medical consenters to make healthcare decisions for the child. The two primary medical consenters are usually the child's caregivers or a caseworker and another CPS staff. The goal of designating multiple consenters is to ensure that a consenter can be present in person when the child receives treatment. This is particularly important when the child is being prescribed psychotropic medications.
DFPS may choose medical consenters and backup medical consenters who are live-in caregivers with knowledge of the child's medical history and needs:
• Foster parents;
• Relatives;
• CPS caseworkers, supervisors, or other CPS staff;
• Parents whose rights have not been terminated, if in child's best interest.
Medical consenters and backup medical consenters must be individuals, not a facility or a facility's shift staff. DFPS may not choose medical consenters and backup medical consenters who are employees of staffed facilities such as Residential Treatment Centers (RTCs), emergency shelters, or intermediate care facilities for individuals with developmental disabilities. CPS caseworkers are usually designated in these cases.
Once the caseworker designates a medical consenter, and the medical consenter meets training requirements, the caseworker must issue Form 2085-B Designation of Medical Consenter (which provides authorization to consent to medical care) to the medical consenter and backup medical consenter, all of whom must sign the form. The CPS caseworker must consent to medical care until a medical consenter and backup medical consenter have been designated and have signed the form.
When the court names an individual as medical consenter, that person is ultimately responsible for the medical decisions for that child and reports directly to the court.
In some cases, the court allows a youth 16 or 17 years old to be their own medical consenter, if other requirements are met. Tex. Fam. Code § 266.010.
Attorneys ad litem and DFPS staff are required to inform 16 and 17 year-olds in foster care of their right to ask the court whether they can consent to their own medical care. Tex. Fam. Code § 107.003(b)(3) and Tex. Fam. Code § 264.121.
DFPS requires both designated primary medical consenters (including youth designated by the court as their own medical consenter) and backup medical consenters to complete the following two department-approved trainings before being allowed to make medical or healthcare decisions:
• DFPS Medical Consent Training for Caregivers; and
• DFPS Psychotropic Medication Training.
3. Temporary Medical Consenters
There are times when medical consent is required for a youth in foster care and the DFPS staff identified as a medical consenter is unavailable.[117] Temporary back up medical consenters are allowed for all medical reasons, not just psychotropic medication. Temporary back up medical consenters can be identified when primary and back up medical consenters cannot provide consent for the following reasons:
• Timely notice of the appointment was not received;
• They are unable to be present due to illness or unforeseen circumstances; or
• An emergency existed where immediate treatment is needed and a delay in medical or psychiatric care could put the child in danger.
In these instances, DFPS and SSCC staff members may be identified as temporary medical consenters to medical treatment, hospital admission, and prescription medications. To provide this consent, they must prepare for the appointment by reviewing the child's condition, current medications, and response to treatment.
4. Informed Consent for Psychotropic Medications
Texas law requires the medical consenter to attend all appointments with the healthcare provider when a child may be prescribed psychotropic medication. The medical consenter must always have a complete discussion with the child's healthcare provider in order to consider options for the child or youth that do not involve medication before or at the same time as using psychotropic medication. According to Texas law, consent to giving a psychotropic medication is valid only if:
• It is given voluntarily and without undue influence, and
• The consenter receives information (given verbally or in writing) describing:
◦ the specific condition to be treated;
◦ the beneficial effects on that condition expected from the medication;
◦ the probable health and mental health consequences of not consenting to the medication;
◦ the probable clinically significant side effects and risks associated with the medication;
◦ the generally accepted alternative medications and non-pharmacological interventions to the medication, if any; and
◦ the reasons for the proposed course of treatment. Tex. Fam. Code § 266.0042.
Texas law requires medical consenters to assure that the child prescribed a psychotropic drug has an office visit with the prescribing healthcare provider at least once every 90 days to allow the practitioner to:
• Appropriately monitor for side effects of the medicine;
• Decide whether the medicine is helping the child; and
• Decide whether continuing the medicine is recommended for the child. Tex. Fam. Code § 266.011.
The medical consenter must attend these medical appointments with the child and provide documentation of the medical appointment to the caseworker by the next business day.
5. Guidance for Youth Who are Their Own Medical Consenter
If a court determines that a youth is capable of consenting to their own medical care, the caseworker must:
• Educate the youth about their medical care and the process for making informed decisions on an ongoing basis;
• Ensure the youth completes the DFPS Medical Consent Training for Caregivers;
• Ensure a youth who has been prescribed psychotropic medication, or is considering taking psychotropic medication, completes the DFPS Psychotropic Medication Training; and
• Offer ongoing support and guidance to the youth.
Before reaching age 16, DFPS must advise the youth of the right to request a hearing to determine whether the youth may be authorized to consent to their own medical care. DPFS provides the youth with training on informed consent and the provision of medical care as part of the Preparation for Adult Living (PAL) program. Tex. Fam. Code § 266.010(l).
Youth in DFPS conservatorship who are not authorized by the court to be their own medical consenters at age 16 or 17 will become their own medical consenters when they turn 18. Conservatorship caseworkers must ensure that 17-year-old youth complete the DFPS Medical Consent Training for Caregivers and DFPS Psychotropic Medication Training if the youth have prescription psychotropic mediations, no later than 90 days before becoming 18 years of age.
Tex. Fam. Code § 264.121(g) requires DFPS to ensure that the youth's transition plan includes provisions to assist the youth in managing the use of any medication and in managing the child's long-term physical and mental health needs after leaving foster care, including provisions that inform the youth about:
• The use of the medication;
• The resources that are available to assist the youth in managing the use of the medication;
• Informed consent; and
• The youth's right to request to be their own medical consenter. Tex. Fam. Code § 264.121(g)(1).
For youth 17 years or older taking medication, DFPS must ensure the youth's transition plan includes a program supervised by a healthcare professional to assist the youth with independently managing their medication. Tex. Fam. Code § 264.121(g)(2).
The youth's caseworker and caregivers should help the youth get information about any medical condition(s), tests, treatment, and medications, and support them in making informed decisions.
If a youth's healthcare decision puts the youth at risk of harm, the court can overrule a youth's decision to refuse medical care even after authorizing the youth to make medical decisions. To do so, the court must find by clear and convincing evidence that the medical care is in the best interest of the youth and also find one of the following:
• The youth lacks the capacity to make the decision;
• Not getting the care will result in observable and material impairment of growth, development, or functioning of the youth; or
• The youth is at risk of causing substantial bodily harm to self or others. Tex. Fam. Code § 266.010(g)(1)-(3).
In these situations, DFPS may file a motion asking the court to order a specific medical treatment or to allow DFPS to consent to medical care for the youth. The motion must include the youth's reasons for refusing medical care and a statement signed by the physician explaining why medical care is necessary. Tex. Fam. Code § 266.010(d)-(e).
6. Assumption of Financial Responsibility by Medical Consenters
During the 89th Regular Legislative Session, a bill added Tex. Fam. Code § 266.0043 providing for the authority of child's medical consenter to access and obtain certain care, to include behavioral health services, for foster children. Effective September 1, 2025, a person, other than DFPS, who is authorized by a court to consent to medical care for a child in foster care, may assume financial responsibility for medical care, including behavioral health services, provided to a child in foster care by an out-of-network provider engaged by the medical consenter on behalf of the child. For that purpose, assuming financial responsibility may include the medical consenter enrolling the child in a health insurance plan. DFPS would not be liable for the cost of such care, unless a court orders DFPS to cover the cost of the medical care. The assumption of financial responsibility authorized by this section of the family code may not be construed to:
• Limit or restrict a foster child's access to Medicaid benefits, including in-network benefits provided under the Medicaid managed care program;
• Change or limit the rights of parents of children in the temporary managing conservatorship of DFPS; or
• Limit a court's authority to order DFPS to assume financial responsibility for the cost of services provided to a foster child by an out-of-network provider.
A medical consenter is required, not later than the 10th business day after the date medical care for which the consenter assumes financial responsibility is provided, to notify the child's caseworker of the provision of that care in the form and manner prescribed by DFPS. DFPS is required to ensure the child's health passport included records of the medical care provided.
A Medicaid Managed Care Organization (MCO) is prohibited from taking adverse action to prevent or discourage a recipient from accessing health care and related services and benefits in accordance with Tex. Fam. Code § 266.0043. STAR Health program managed care is required to contract between a Medicaid MCO and the Health and Human Services Commission to require that the MCO comply with that prohibition against taking adverse action. Nothing can be construed to confer liability on a Medicaid MCO for the cost of health care and related services provided to a child in foster care by an out-of-network provider engaged by a medical consenter on behalf of the child. Tex. Govt. Code § 540.0807.
G. Admission of a Child in DFPS Custody to an Inpatient Mental Health Facility
DFPS may request admission to an inpatient mental health facility only if a physician states that the child has a mental illness or demonstrates symptoms of a serious emotional disorder and presents a serious risk of harm to themselves or others. Tex. Health & Safety Code 572.001. DFPS may not admit a child in DFPS conservatorship to an inpatient mental health facility based on the child's consent to be admitted.
The admission is considered a significant event for purposes of Tex. Fam. Code § 264.018 and requires notice to all parties entitled to notice and to the court of continuing jurisdiction within three days of admission. DPFS must continue to review the need for continued placement and if DFPS determines there is no longer a need for inpatient treatment, DFPS must notify the facility administrator that the child may no longer be detained without an application for court-ordered mental health services.
H. Monitoring Psychotropic Medications
In February 2005, DFPS, the Department of State Health Services (DSHS), and the Health and Human Services Commission (HHSC) released a "best practices" guide to ensure the proper use of psychotropic medications for the children in foster care.
The Psychotropic Medication Utilization Parameters for Children and Youth in Texas Public Behavioral Health: Medication Tables (7th version)[118] are the most recent versions of these guidelines. They serve as a resource for physicians and clinicians who care for children diagnosed with mental health disorders. The guides provide recommendations for the appropriate use of psychotropic medications for children served by the public behavioral health system in Texas, including those in foster care, and includes nine criteria indicating the need for review of the child's clinical status.
Since April 2008, STAR Health has conducted PMURs on the children whose medication treatment fall outside of the expectations of the Parameters.
PMUR Process for STAR Health Members FAQ and Stakeholder Manual explains this process and how to request a review.[119] Please also see the Psychotropic Medication chapter of this Bench Book.
I. End of Life Medical Decisions
If a child in DFPS conservatorship has been diagnosed with an “irreversible condition” or a “terminal condition” and medical professionals suggest withholding or withdrawing life-sustaining treatment, the regular process for medical consent does not apply and the caseworker and supervisor must follow the procedures outlined below. However, any party may seek court intervention at any time if all parties do not agree on a course of action or if any party is concerned about the child's rights. CPS Policy Handbook § 11720.
If parental rights have not been terminated and the child's attending physician recommends end-of-life care, the parents have the authority to make the end-of-life decisions even if DFPS is the temporary managing conservator (TMC) or permanent managing conservator (PMC) of the child. DFPS staff or other medical consenters do not have the legal authority to consent in these circumstances. CPS Policy Handbook § 11721.
If parental rights have been terminated as to both parents, or the parents are deceased and the attending physician recommends end-of-life care, the caseworker and supervisor must:
• Obtain a written statement from the attending physician certifying that the child has a terminal or irreversible condition, and that the physician recommends withholding or withdrawing life-sustaining treatment;
• Request a second opinion or a review by a hospital medical or ethics review board if there are any concerns regarding the recommendation of the attending physician;
• Confirm that there is no relative, fictive kin, or other individual with possessory or custodial rights of the child. If one of these individuals is available, that person must be consulted for end-of-life decisions, if possible;
• Notify and discuss the recommendation with the program director, regional director, regional attorney, attorney representing DFPS, the child's attorney ad litem, guardian ad litem, CASA (if applicable), and any other legal party to the case; and
• Notify and consult with the court of continuing jurisdiction. CPS Policy Handbook § 11722.
J. Health Passport
The Health Passport is a web-based, secure health information tool which utilizes claims data to provide information on healthcare services for every child, youth, or young adult enrolled in the STAR Health program. The Health Passport is not a full medical record. It contains the following information:
• A record of healthcare visits and services with any network provider;
• Immunizations, lab results, and prescriptions received;
• Healthcare forms such as psychotropic reviews, service plans, Texas Health Steps forms, CANS results, and the FSNA;
• Allergies, vital signs, height, weight, and record of future scheduled appointments if entered by network providers;
• A two-year history from prior to entering foster care if the child received Medicaid or Children's Health Insurance Program (CHIP) coverage in the past; and
• Name and phone number of the STAR Health Service Coordinator.
Medical consenters, caseworkers, network providers, some CASA staff, and some residential provider staff are able to view Health Passport records. STAR Health Network providers are able to enter data into Health Passport.
Only a DFPS staff member may give a printed copy of the Health Passport or sections of the Health Passport to other persons or entities, including judges.
K. Court Orders for Medical Services
If a healthcare professional has been consulted regarding a healthcare service, procedure, or treatment for a child in DFPS conservatorship, a court must make findings in the record supporting its decision if the court declines to follow the recommendation of the healthcare professional. Tex. Fam. Code § 266.005.
Special Issue: If the child needs a service not covered by Medicaid, the judge may order that a physician assess the need for the service if that has not already been done. Also, the judge may order the service and DFPS will seek that service through a private pay contract. When entering orders for services that are not covered by Medicaid, a judge might consider drafting an order that provides DFPS the maximum flexibility in contracting because a particular provider may not be in the position to fulfill the contract as dictated by the court order. Also, a copy of the signed order should be sent via fax to Superior HealthPlan at 1-866-702-4837 or the court order can be escalated through the DFPS Well-being Specialist who works directly with the STAR Health Liaison.
STAR Health is required to pay for Medicaid covered services ordered by a court pursuant to the statutory citations listed below. STAR Health cannot deny, reduce, or controvert the court's orders for Medicaid inpatient mental health covered services for members from birth through age 20, when such inpatient mental health services are provided pursuant to:
• A court order; or
• As a condition of probation.
STAR Health cannot deny, reduce, or controvert the court orders for Medicaid inpatient mental health covered services for members of any age if the court-ordered services are delivered in an acute care hospital.
STAR Health may not limit substance use disorder treatment or outpatient mental health services for members of any age provided pursuant to:
• A court order; or
• A condition of probation.
STAR Health cannot apply its own utilization management criteria through prior authorizations, concurrent reviews, or retrospective reviews for such services. Any modification or termination of services must be presented to the court with jurisdiction over the matter for determination. A member who has been ordered to receive treatment pursuant to a court order can only appeal the court order through the court system. STAR Health is required to have a mechanism to receive court order documents from providers at the time of an authorization request.
STAR Health must provide all Medicaid inpatient psychiatric covered services to members and outpatient covered services to members of any age who have been ordered to receive the services by:
• A court of competent jurisdiction including services ordered pursuant to the Tex. Health & Safety Code Chapters 573, Subchapters B and C, Tex. Health and Safety Code Chapter 574, Subchapters A-G, Tex. Fam. Code 55, Subchapter D; or
• As a condition of probation.
Federal statute prohibits Medicaid funding for services delivered to Medicaid members ages 21-64 years of age while residing in an IMD. For STAR Health members ages 21 years of age or older, STAR Health may provide inpatient services for acute psychiatric conditions in a free-standing psychiatric hospital for up to 15 days per calendar month in lieu of an acute care inpatient hospital setting as allowed by 42 C.F.R. § 438.6(e).
STAR Health must provide Medicaid-covered substance use disorder treatment services, including substance use disorder residential treatment services, required as a court order consistent with Tex. Health and Safety Code Chapter 462, Subchapter D, or as a condition of probation.
These requirements are not applicable when the member is considered to be incarcerated.
L. References
Key STAR Health Phone Numbers
|
Organization |
Phone Number |
|
Superior HealthPlan Member Services Hotline |
1-866-912-6283 |
|
1-866-566-8989 |
Nonemergency Medical Transportation Services
Nonemergency Medical Transportation[120] (NEMT) services provide medical transportation services for youth who do not have a way to get to covered healthcare services. NEMT services allow the youth to arrange a ride to a doctor's office, dentist's office, hospital, drug store, or any place that provides covered healthcare services. Types of rides and related covered expenses include:
• Public transportation (for example, the city bus);
• A taxi, ride share, or van service;
• Commercial transit, like a bus or plane, to go to another city for an appointment;
• Money for gas;
• Meals and lodging for children and youth age 20 years and younger staying overnight to get covered healthcare services; and
• Payment for some out-of-state travel.
If STAR Health youth need medical transportation services, it is recommended to contact the SafeRide Appointments/Call Center at 1-855-932-2318; TTY: 7-1-1. Additionally, the “Where's My Ride" line at 1-855-932-2319; TTY: 7-1-1 is available to schedule a return ride home from an appointment or to check on the status of a scheduled ride. If there is a complaint about services, it is recommended to contact the phone number on the back of the member ID card.
M. Who to Contact with Health Care Questions
DFPS developed a STAR Health mailbox which is staffed by the DFPS medical services team and is checked each business day. The email address is: DFPSStarHealth3In30@dfps.texas.gov.
Superior STAR Health staff are also available to serve as a liaison to help court teams navigate through the STAR Health program and avoid gaps in care and services to children and youth. Superior STAR Health can help court teams:
• Facilitate interactions between Superior STAR Health, caseworkers, and Child-Placing Agencies to provide a single point of contact.
• Access to Superior STAR Health Liaisons who conduct education and provide court teams and caregivers with customized information packets.
• Enhance communication with court teams and Superior STAR Health pertaining to referrals and follow-up for improved accountability, collaborative efforts and streamlined resolutions.
• Collaborate with Court Teams to achieve better outcomes for members and foster parents.
• Offer Superior STAR Health benefits education including, but not limited to, the 24/7 Nurse Advice Line and NEMT options through the Superior STAR Health training team.
• Obtain assistance from Superior Member Advocates with Medicaid-related needs and barriers Court Teams identify by calling 1-866-912-6283.
• Address pending needs and resources during the staffing that occurs outside of court proceedings.
• Follow identified cases until referrals are completed and members are linked with appropriate services.
• As of 9/1/23, all STAR Health members are assigned a service coordinator.
To set up a court meeting and training, provide the following information by email to Superior STAR Health at SH_JudicialMailbox@superiorhealthplan.com.
• Your name;
• Your contact number;
• Your email address; and
• What Superior STAR Health can assist you with.
Additional Links / Resources:
• Texas DFPS Star Health webpage[121]
• Superior HealthPlan STAR Health website[122]
Children with Disabilities
Introduction
A. What Laws and Policies Protect Individuals with Disabilities?
A number of federal laws protect individuals with disabilities from discrimination in public and private settings. Some of these laws include:
• The Americans with Disabilities Act (ADA) 42 U.S. Code § 12101 et seq., which prohibits discrimination on the basis of disability in employment, state and local government, public accommodations, commercial facilities, transportation, and telecommunications;
• The Rehabilitation Act of 1973, which prohibits discrimination by any entity that receives federal funds;
• The Individuals with Disabilities Education Act (IDEA) 20 U.S.C. § 1400, et. seq., which requires states to provide students with disabilities special education and related services;
• The Fair Housing Act 42 U.S.C. § 3601 et seq. which addresses discrimination in housing;
See Guide to Disability Rights Laws for a summary of federal laws.[123]
B. Children with Disabilities in DFPS Care
Children with disabilities in DFPS conservatorship must be provided with a placement and services to meet their needs.
The Home and Community-based Services (HCS) Medicaid Waiver program provides comprehensive, individualized community-based services to individuals with intellectual and developmental disabilities, including to children within DFPS conservatorship who qualify, so that they can live in the community.
Please note that an individual must still meet general eligibility criteria for the HCS program as well as the specific criteria below.
|
Source of HCS Slot |
Eligibility Criteria |
Process to Access |
|
DFPS Aging Out of Care (AOC) |
▪ Close to aging out of conservatorship (age 16 or older) and in need of continued care beyond age 18. ▪ Live in a foster home or a residential facility. Note: the youth cannot continue to live in a residential facility once enrolled in the HCS waiver. ▪ There are a very limited number of these slots so they should not be used for youth who can access. another type of waiver or the HCS waiver using a different slot type. |
▪ When the transition plan is staffed at age 16, DFPS Developmental Disability Specialist (DDS) determines if an HCS slot is needed. ▪ The Developmental Disability Specialist (DDS) completes referral forms and submits to DFPS state office where referrals are prioritized based on situation and age. ▪ Contact: Developmental Disabilities Program Specialist, State Office |
|
Promoting Independence (PI) |
▪ Any age. ▪ Registered on the HCS interest list. ▪ Reside in a large, private ICF-MR. Large is defined as 14 or more beds. |
▪ HHSC offers HCS slots to individuals who are residents of large ICFs-MR and on the HCS interest list. HCS slot offers are made to these individuals to ensure these individuals move within 365 days of being registered on the PI list. If the slot is turned down, HHSC ensures the youth remains on the PI list. CPS staff should secure guidance from the DDS before accepting or declining an HCS slot as other services may be impacted. ▪ The DDS may also request that the ICF-MR conduct a staffing to determine if another “living option” is appropriate. |
|
Small/Medium Intermediate Care Facility (ICF-MR) Rider |
▪ Under the age of 22. ▪ Reside in a small, private ICF-MR (6 beds) or a medium, private ICF-MR (7-13 beds). ▪ There are very few of these slots available. |
▪ HHSC offers slots based on an individual's interest list date. ▪ The DDS may also request that the ICF-MR conduct a staffing to determine if another “living option” is appropriate. |
|
Money Follows the Person (MFP) |
▪ Under the age of 22 for Home and Community Based Services (HCS). ▪ Residing in a nursing facility. ▪ Note: Money Follows the Person (MFP) also applies to other Medicaid Waivers: Community Living Assistance and Support Services (CLASS) (any age), Medically Dependent Children Program (MDCP) (under 21), Community Based Alternatives (CBA) (21 or older), and Deaf-Blind Multiple Disabilities (DB-MD) (18 or older). |
▪ HHSC conducts the Permanency Planning process every 6 months for residents in nursing facilities. Alternative services/options are discussed and if placement into the community is desirable, the MRA notifies HHSC requesting an HCS slot. After age 22 this option ends. |
|
State Supported Living Center |
▪ Residing in a State Supported Living Center. |
▪ The Service Planning Team (SPT) at the facility determines if and when an individual is referred for community placement. Once the SPT makes that determination, HHSC offers an HCS slot to that individual and community placement must occur within 6 months. ▪ The DDS can request a “living option” staffing at any time. ▪ The decision to accept an HCS slot is ultimately made by either DFPS or the guardian if there is one. |
|
State Hospital Multiple Disability Unit (MDU) |
▪ Committed to a state mental health hospital. |
▪ Upon admittance, the DDS can request that HHSC put the youth on the MDU HCS waiting list; wait time for a slot varies and discharge from the hospital may be required before a slot is available. |
|
Interest List |
▪ HHSC determines eligibility when the individual's name comes to the top of the list. |
▪ DDS should put any child they suspect may have a disability on the interest lists for all waivers at the time the child comes into care. This is important to do even if the goal for the child is reunification as waivers are an important resource for birth families. ▪ Contact: local LIDDA office |
DFPS Developmental Disability Specialists are the main point of contact for information about serving children with disabilities in the child welfare system. Responsibilities for the Developmental Disability Specialist are outlined in the CPS Policy Handbook § 6411.31 Responsibilities of the Developmental Disability Specialist and CPS Policy Handbook § 6411.4 Children with Primary Medical Needs and Special Health Care Needs.
Relevant CPS Policy Handbook sections include:
• 4117 Specific Placement Considerations for Children or Youth Who Have Primary Medical Needs
• 4118 Additional Actions for Placing Children with Intellectual or Developmental Disabilities
• 4131.1 Durable Medical Equipment
• 6237 Permanency Planning for Children with Intellectual or Developmental Disabilities in Institutional Settings
• 10340 Preparation for Long-Term Care or Support in Adulthood for Youth with Disabilities
• 1570 Supplemental Security Income (SSI) for Children in Foster Care
• 10341.2 Ensuring Funding and Eligibility for Services
• 1543 Payment for Long-Term Care in Adulthood
Relevant DFPS Resource Guides include:
• Mental Health Resource Guide
• Education for Children Resource Guide
• Preparation for Long Term Care and Support Resource Guide
Additional educational information on IDD and HCS placements can be accessed in the archived May 2025 webinar on Representing Children with Intellectual and Developmental Disabilities in Child Welfare Cases and the related Power Point and Medicaid Waiver Comparison Chart.
C. Benefits from the Social Security Administration
1. Child receives income from Supplemental Security Income (SSI) or Retirement, Survivors, and Disability Insurance (RSDI)
A child entering DFPS conservatorship may be entitled to various benefits through the Social Security Administration (SSA).[124] If the child is currently receiving benefits, DFPS must promptly notify SSA that the child is under DFPS conservatorship so that DFPS can apply to become the representative payee of the child's benefits.[125] Once SSA approves DFPS to be the child's representative payee, DFPS will generally remain the payee until DFPS conservatorship ends or until the young adult exits extended foster care. Regional SSI Coordinators oversee this process of applying for the transfer to DFPS as the representative payee. When a child or young adult exits foster care or extended foster care, the child's caregiver or the young adult must go to an SSA office to request the transfer of SSI or RSDI benefits to the caregiver or the young adult as payee.
Special Issue: Obtaining transportation to this appointment can help to ensure that the benefits transfer to the young adult is successfully completed.
2. SSI for a child in traditional foster care
Children in foster care may qualify for the federal benefit of Supplemental Security Income due to a mental or physical disability. Supplemental Security Income (SSI) is available to children with disabilities who have limited income and resources. For a child in foster care, the DFPS SSI Coordinator may apply for SSI benefits for a child who is also eligible for Title IV-E foster care assistance. If DFPS claims Title IV-E foster care assistance for the child's maintenance payment, DFPS cannot use the child's SSI benefit to offset the Title IV-E foster care payment.[126]
Special Issue: The decision to apply for SSI while a child is in foster care is based upon the amount of the child's foster care payment. The regional eligibility specialist should be consulted with questions regarding funding reimbursement.
3. SSI for a child in a relative or kinship placement
DFPS does not make foster care payments to non-licensed relatives or kinship caregivers but sends the SSA benefits to these caregivers to meet the child's daily needs. The SSI coordinator asks SSA to reinstate the child's SSI benefits when the situation meets both of the following criteria:
• SSA had suspended the child's SSI benefits due to Title IV-E eligibility.
• The child is placed with a non-licensed relative or kinship caregiver. CPS Policy Handbook § 1571.2 Changes that Affect Claiming SSI or Title IV-E Benefits.
The caseworker should contact the DFPS regional SSI Coordinator to inquire about applying for Social Security benefits.[127]
4. SSI Applications for youth aging out of care
While under the conservatorship of DFPS, the SSI Coordinator submits SSI applications on behalf of the youth. Under DFPS policy, if a youth in care has a disability and may be eligible for SSI, the DFPS caseworker should contact the regional SSI Coordinator to discuss applying when the youth turns 17 years old. Since youth may not meet the adult definition of disability,[128] SSI applications should be filed well before a youth's 17th birthday to prevent delay in application processing and additional delays if an unfavorable decision needs to be appealed.
Special Issue: It is critical for youth to have their funding source switched before they age out, so youth should apply for SSI by age 16 to avoid delay with waitlists. For youth who have not had SSI before, the process can be very lengthy.
SSA requires each SSI recipient or potential recipient who is 18 years old to be evaluated according to adult listing of impairments.[129] Aside from individual identification, DFPS state office sends a quarterly report to regional SSI coordinators identifying youth in foster care who are 17 years old and are potentially eligible for SSI, regardless of their eligibility for Title IV-E assistance.[130]
5. Preserving SSI benefits for young adults in extended foster care
Young adults in extended foster care may continue to receive SSI benefits, but the payments will continue to be paid to DFPS. However, young adults in extended foster care must be aware and mindful of factors that could make them ineligible to continue receiving benefits. For example, the young adult may not accumulate more than $2,000 in cash assets or their benefit payment may be reduced or terminated; young adults who may also be working, receiving scholarships, or have some other income (such as annuity payments) need to be educated and reminded to notify DFPS of any income they receive and may have to inform DFPS of funds in any bank accounts they have. Once a young adult exits extended foster care, they must go to an SSA office to request to become their own payee. Young adults may consider applying for an ABLE Account in which to place funds that may make them ineligible to continue receiving SSI benefits.[131] Another option for preserving benefit eligibility is a Master Pooled Trust account through the Arc of Texas.
D. Parents and Other Adult Caregivers with Disabilities and Child Welfare
Federal law prohibits governmental agencies, including child welfare and court systems, from discriminating against people with disabilities in their services, programs, and activities. Agencies in the child welfare system must provide accommodations to ensure persons with disabilities have equal opportunity to access services to ensure safety, permanency, and well-being for the children and families DFPS serves.
See the DFPS Resource Guide – Working with Persons with Disabilities for information on working with persons with disabilities in the child welfare system, including specific suggestions for reasonable accommodations for a parent with a disability when child safety is involved.
E. What Resources are Available for Children and Adults with Disabilities?
• Special Needs Training for Parents and Caregivers[132]
• Disability Rights Texas (DRTx) provides legal representation and advocacy for individuals with disabilities.[133] DRTx can help caregivers and caseworkers advocate for services for a child with disabilities in the school system, appeal denials of Medicaid services, or advocate for other community-based services, or may be appointed as a child's ad litem in limited counties.
• EveryChild Inc. provides assistance and support for children with disabilities to reside in a family setting.[134]
• Texas Health and Human Services Disability webpage includes disability-related resources and information.[135]
• Home and Community-based Services (HCS) is a Medicaid waiver program that provides services and support for individuals with intellectual disabilities.[136]
• The Judicial Commission on Mental Health Texas Mental Health and Intellectual and Developmental Disabilities Law Bench Book is a procedural guide for Texas judges hearing cases regarding persons with mental illness and/or intellectual and developmental disabilities (IDD).[137]
• Local Intellectual and Developmental Disability Authorities (LIDDA) and Local Mental Health Authorities (LMHA) support children and adults in crisis. Local LIDDA and LMHA contacts are available on the Texas Health and Human Services webpage at Contact HHS webpage.[138]
• Navigate Life Texas is a website developed by HHS to explain resources for families with children who have disabilities and special health care needs.[139]
Psychotropic Medication
Introduction
Psychotropic medications are substances that affect the mind and alter mental processes, such as perception, mood, and behavior. Psychotropic drugs include stimulants, antidepressants, antipsychotics, and mood stabilizers. Some children need to use psychotropic medications long-term to treat mental health disorders that they inherited or developed, such as attention deficit hyperactivity disorder (ADHD), major depressive disorder, or psychosis. Other children need to use psychotropic medications on a more temporary basis to help relieve severe emotional stress and help them function in school, at home, and in the community.
The use of psychotropic medication in children in foster care may be life-saving and relieve challenging and sometimes severe symptoms of mental health disorders. Children and youth in foster care may benefit from medication to address mental illness exacerbated by the effects of trauma brought on from exposure to abuse or neglect. However, studies have shown that psychotropic medications can have serious side effects on adults using them, and the effects of long-term use in children and adolescents remain largely unknown. Some psychotropic medications do not have Food and Drug Administration (FDA) approved labeling for use in children.[140] Therefore, it is imperative that a comprehensive evaluation be performed before beginning treatment with psychotropic medication for a mental, emotional, or behavioral disorder. Except in the case of an emergency, a child should receive a thorough health history, biopsychosocial assessment, mental status exam, and physical exam before being prescribed a psychotropic medication.[141]
Under Tex. Fam. Code § 266.001, a “psychotropic medication” means a medication that is prescribed for the treatment of symptoms or psychosis or another mental, emotional, or behavioral disorder and that is used to exercise an effect on the central nervous system to influence or modify behavior, cognition, or affective state. The term includes the following categories when used as described by Tex. Fam. Code § 266.001(7):
• Psychomotor stimulants;
• Antidepressants;
• Antipsychotics or neuroleptics;
• Agents for control of mania or depression;
• Anti-anxiety agents; and
• Sedatives, hypnotics, or other sleep-promoting medications. Tex. Fam. Code § 266.001(7).
Texas led the nation in creating oversight protocols in 2005 when the 79th Texas Legislature enacted Senate Bill 6. This sweeping legislation proposed reforms for DFPS, including a plan to place all children and youth in foster care under a single comprehensive managed care system. Texas was the first state to develop a "best practices" guide for oversight of psychotropic medications for children in foster care. Released in 2005 and most recently updated in July 2025, DFPS, the Department of State Health Services (DSHS), and the Health and Human Services Commission (HHSC) developed the Psychotropic Medication Utilization Parameters for Children and Youth in Texas Public Behavioral Health (7th Edition) (Parameters).[142] The Parameters are updated periodically and serve as a resource for physicians and clinicians who care for children diagnosed with mental health disorders.
Additionally, DFPS' Behavioral Health Services Division includes a Behavioral Health Services Division Administrator, a Trauma-Informed Care Manager, six regional Trauma-Informed Care Program Specialist positions, a Behavioral Health Program Specialist Lead position, three Substance Use Program Specialists, two Child and Adolescent Needs and Strengths (CANS) Program Specialists, and three Mental Health Program Specialists. For more information about this division, see the Substance Use Disorders chapter of this Bench Book.
The Texas Legislature also enacted Tex. Fam. Code Chapter 266 which governs medical care and education services for children in foster care primarily through three processes:
• Medical Consenter;
• Agency Oversight; and
• Judicial Review.
A. Medical Consenter
Tex. Fam. Code § 266.004(h) requires medical consenter training, which must include training related to informed consent for the administration of psychotropic medication and the appropriate use of psychosocial therapies, behavior strategies, and other non-pharmacological interventions that should be considered before or concurrently with the administration of psychotropic medications. Tex. Fam. Code § 266.004(h-1).
Each person required to complete a training program under Tex. Fam. Code § 266.004(h) must acknowledge in writing that the person:
• Has received the training described by Tex. Fam. Code § 266.004(h-1);
• Understands the principles of informed consent for the administration of psychotropic medication; and
• Understands that non-pharmacological interventions should be considered and discussed with the prescribing physician, physician assistant, or advanced practice nurse before consent to the use of a psychotropic medication. Tex. Fam. Code § 266.004(h-2).
The DFPS Medical Consent Training for Caregivers is available online and typically takes an estimated two and half hours to complete.[143]
DFPS also has a two-hour online Psychotropic Medication Training for DFPS staff, foster parents and residential providers, relative caregivers, and youth medical consenters.[144]
1. Informed Consent
Although the term “informed consent” as it relates to medical care for a child in foster care is not defined in Tex. Fam. Code Chapter 266, the Texas Legislature has defined consent for psychotropic medication. Consent to the administration of a psychotropic medication is valid only if:
• The consent is given voluntarily and without undue influence;
• The person authorized by law to consent for the foster child receives verbally or in writing information that provides:
◦ the specific condition to be treated;
◦ the beneficial effects on that condition expected from the medication;
◦ the probable health and mental health consequences of not consenting to the medication;
◦ the probable clinically significant side effects and risks associated with the medication; and
◦ the generally accepted alternative medications and non-pharmacological interventions to the medication, if any, and the reasons for the proposed course of treatment. Tex. Fam. Code § 266.0042.
The Parameters describe what is meant by “informed consent” by stating that consent to medical treatment in non-emergency situations must be obtained from appropriate parties with the child or adolescent assenting before beginning psychotropic medication, which includes discussing the following with the prescribing provider before consenting:
• A DSM-5 (or current edition of the American Psychiatric Association's [APA] Diagnostic and Statistical Manual of Mental Disorders) psychiatric diagnosis for which the medication is being prescribed;
• Target symptoms;
• Expected benefits of treatment;
• Risks of treatment, including common side effects, laboratory finding, and uncommon but potentially severe adverse events;
• Risks of no treatment; and
• Alternative treatments available and/or attempted treatments.[145]
Included in the idea of informed consent is the consideration of alternative treatments and trauma-informed care. The concept of trauma-informed care is a paradigm shift for the entire system and acts as a lens through which children, youth, and families experiencing the child welfare system are viewed. The Introduction and General Principles Section of the Parameters promote a trauma-informed child and family-serving system where all parties involved recognize and respond to the varying impact of traumatic stress on those who have contact with the system, including youth, caregivers, and service providers. A robust trauma-informed system should not only screen for trauma exposure and related symptoms, but also use culturally and linguistically appropriate, evidence-based assessments and treatment.
In 2015, the 84th Texas Legislature added Tex. Fam. Code § 266.012 regarding comprehensive assessments. Described in detail in the Health Care chapter herein, the comprehensive assessment for children and youth in state conservatorship is called CANS and is administered in a developmentally appropriate way not later than the 45th day after the date a child enters the conservatorship of DFPS. This statute was updated in 2017 to require that any Single Source Continuum Contractor (SSCC) providing therapeutic foster care services to a child ensure that the child receives a comprehensive assessment at least once every 90 days. Tex. Fam. Code § 266.012(c). The assessment must include:
• A screening for trauma; and
• Interviews with individuals who have knowledge of the child's needs. Tex. Fam. Code § 266.012(a).
DFPS requires that children and youth placed in substitute care ages 3 to 17 years old receive a CANS assessment within 30 days of removal. The CANS is used to gather information about the strengths and needs of the child and family and is used in Service Planning to assist the child and family in reaching their goals.[146] DFPS may consent to healthcare services ordered or prescribed by a healthcare provider authorized to order or prescribe healthcare services regardless of whether services are provided under the medical assistance program under Tex. Hum. Res. Code Chapter 32, if DFPS otherwise has the authority under Tex. Fam. Code § 266.004 to consent to healthcare services. Tex. Fam. Code § 266.004(k).
2. Monitoring Use of Psychotropic Drugs
The medical consenter shall ensure that the child has been evaluated by the prescribing physician, physician assistant, or advanced practice nurse at least once every 90 days to allow the physician, physician assistant, or advanced practice nurse to:
• Appropriately monitor the side effects of the medication; and
• Determine whether:
◦ the medication is helping the child achieve the treatment goals; and
◦ continued use of the medication is appropriate. Tex. Fam. Code § 266.011.
B. Agency Oversight
The Parameters provide recommendations for the appropriate use of psychotropic medications for children served in the public behavioral health system, including children in foster care. They include criteria indicating the need for review of the child's clinical status. Medical consenters, caregivers, judges, attorneys, and advocates also use the Parameters as they fulfill their duties of advocacy and oversight.
1. Medication Review
The STAR Health managed care organization (MCO) oversees automated reviews of pharmacy claims data for all children in foster care receiving psychotropic medications to identify medication treatments which appear to be outside the Parameters. Additionally, STAR Health MCO clinical staff routinely conduct telephonic health screenings when children newly enter DFPS conservatorship or change placements.
The telephonic health screening includes screening of the child's psychotropic medications treatment. The screening process includes criteria such as:
• Does the child have a documented mental health diagnosis?
• What is the child's age? (Prescriptions might need further review if the child is under age 3 or 4, depending on the class of medication.)
• Is the child taking two or more medications from the same drug class? (Two mood stabilizers and long and short acting stimulants from the same “family” are allowed, but two or more medications from the same class call for further review.)
• Is the child prescribed four or more psychotropic medications regardless of the class?
2. Psychotropic Medication Utilization Review [147]
The Psychotropic Medication Utilization Review (PMUR) process is designed to determine whether a child's psychotropic medication treatment is outside of the Parameters and, if so, whether a consultation call from a STAR Health child psychiatrist to the prescribing physician is indicated. A PMUR can be initiated by the STAR Health MCO if indicated by a health screening or pharmacy claim review. A PMUR may also be triggered by a request from any judge, attorney, caseworker, advocate, foster parent, medical consenter, or other concerned person working with the child. The PMUR examines child-specific clinical information about a child's diagnoses, medication dosage, and whether the medication treatment is in compliance with the Parameters. The STAR Health MCO has committed to prioritize responses to inquiries from judges concerning children under their supervision. PMUR findings are usually sent to the child's caseworker or can be faxed or emailed directly to the court, if requested.
All PMUR requests are reviewed by one of five STAR Health Licensed Behavior Health Clinicians who gather medical records and screen children's psychotropic medication treatment for compliance with the Parameters. If the treatment is outside the Parameters, the clinician refers the case to a STAR Health child psychiatrist to conduct a PMUR. The child psychiatrist outreaches to the treating physician, works with the treating physician to reduce polypharmacy if indicated, and prepares a PMUR report. The PMUR report will contain a formal determination about the foster child's medication treatment. The possible determinations are as follows:
• Medication treatment within Parameters;
• Medication treatment outside Parameters. Medication treatment reviewed and found to be within the standard of care;
• Medication treatment is outside Parameters and there is opportunity to reduce polypharmacy; or
• Medication treatment is outside Parameters and there is risk for or evidence of significant side effects.
The STAR Health MCO is in a good position to intervene and educate the prescribing physician because it holds a contract with these providers to participate in STAR Health. Physicians and other clinicians who appear to consistently prescribe outside the Parameters despite risk for or evidence of significant side effects, or when there is an opportunity to reduce polypharmacy, are referred to the Quality of Care (QOC) review process. Additional records are examined for pervasive patterns of over-prescribing or dangerous prescribing. Qualifying cases may be referred to the Peer Review Committee for further investigation and action. The Peer Review Committee is established by the MCO and consists of network providers to review PMUR concerns for STAR Health Members that exceed the QOC thresholds. Superior HealthPlan also utilizes consultant physicians as needed to review specific specialist issues if a need is identified. The results of Quality Improvement and Peer Review Committee investigations and actions are confidential and may not be released to or discussed with the public. All QOC issues are tracked and trended. Any practitioner showing a pattern or trend may be placed on corrective action and/or face disciplinary action up to and including termination of contract, if warranted.
A PMUR cannot address whether other medications might be effective, and this process is not the appropriate avenue to address immediate concerns about new medications or medication side effects. Instead, the informed consent process is considered the appropriate avenue to inquire about new medications and side effects. In these situations, the STAR Health MCO recommends that the Medical Consenter contact the prescribing physician directly. DFPS also employs CPS Nurse Consultants in each administrative region to assist CPS staff with children's health issues, including questions about psychotropic medications.
Please see the PMUR Process for STAR Health Members FAQ and Stakeholder Manual for more information on the process.[148]
3. Effect of Texas' Oversight Process
As a result of the various improvements to Texas' oversight process, including hiring a Medical Director at DFPS, implementing the Parameters as a statewide monitoring system, and launching managed care and clinical consultation by the STAR Health programs, the prescription patterns of psychotropic medications for Texas children experiencing foster care have improved significantly. Since implementation of the Parameters in 2005, the use of psychotropic medications in Texas foster care has decreased substantially from a high of 31.4% in 2004 to 17% in 2021 for children prescribed psychotropic medications for 60 days or more.[149] It should be noted in 2020, HHSC revisited the foster care prescription data from State Fiscal Years 2002 to 2021 using the new psychotropic drug list and other methodological changes to provide a single consistent historical timeline. Previous versions of the cited report incorporated changes as they occurred. Due to programming code changes, additional data becoming available, and additional medications being added to the list of psychotropic medications, the data have changed from previous versions of the report.[150] When reviewing the chart below, please note that it contains a new data measurement regarding “any psychotropic medication prescription,” as indicated by the blue line. The use of any children prescribed psychotropic medications in Texas foster care has decreased substantially from a high of 37.7% in 2004 to 23.2% in 2021.
Percentage of Children and Youth in Texas Foster Care
Receiving Psychotropic Medications by Measure*
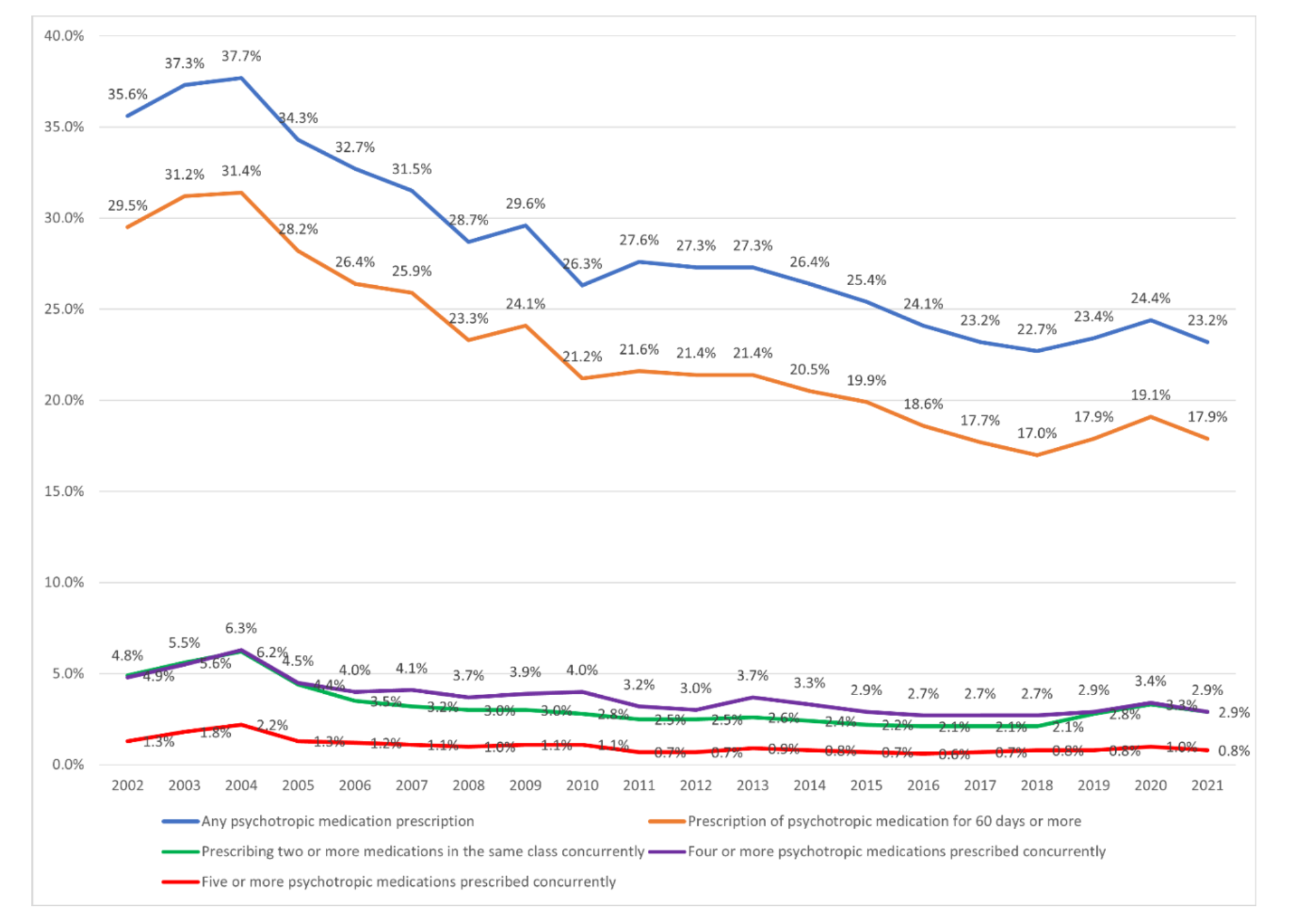
**Please note that psychotropic medications may be used off label for medical reasons.
C. Parental Notification of Certain Medical Conditions
DFPS must provide notice of significant events regarding a child in foster care to the child's biological parents and others under Tex. Fam. Code § 264.018 in a manner that would provide actual notice to a person entitled to the notice, including the use of electronic notice whenever possible. Tex. Fam. Code § 264.018(c).
Not later than 24 hours after an event described by Tex. Fam. Code § 264.018(d), DFPS shall make a reasonable effort to notify a parent of a child in the managing conservatorship of the DFPS and the parent's attorney, if represented by an attorney, of:
• A significant change in medical condition of the child;
• The enrollment or participation of the child in a drug research program under Tex. Fam. Code § 266.0041;
• An initial prescription of a psychotropic medication; and
• A change in the child's placement. Tex. Fam. Code § 264.018(d).
As soon as possible but not later than 48 hours after DFPS becomes aware of a significant event affecting a child in the conservatorship of DFPS, DFPS shall provide notice of the significant event to the child's parent and the parent's attorney, if represented by an attorney. Tex. Fam. Code § 264.018(f).
Under Tex. Fam. Code § 264.018(a)(5), a significant event includes:
• A placement change, including failure by DFPS to locate an appropriate placement for at least one night;
• A significant change in medical condition;
• An initial prescription of a psychotropic medication or a change in dosage of a psychotropic medication;
• A major change in school performance or a serious disciplinary event at school;
• A placement in a qualified residential treatment program, as that term is defined by 42 U.S.C. Section 672(k)(4); or placement in a residential treatment center as defined by Tex. Fam. Code § 263.001, including meetings or conferences to determine the appropriateness of such a placement; or
• Any event determined to be significant under DFPS rule.
For purposes of Tex. Fam. Code § 264.018(f), if a hearing for the child is conducted during the 48-hour notice period, DFPS shall provide notice of the significant event at the hearing. Tex. Fam. Code § 264.018(g).
DFPS is not required to provide notice under Tex. Fam. Code § 264.018 to a parent of a child in the managing conservatorship of DFPS if:
• DFPS cannot locate the parent;
• A court has restricted the parent's access to the information;
• The child is in the permanent managing conservatorship of DFPS and the parent has not participated in the child's case for at least six months despite DFPS' efforts to involve the parent;
• The parent's rights have been terminated; or
• DFPS has documented in the child's case file that it is not in the best interest of the child to involve the parent in case planning. Tex. Fam. Code § 264.018(h).
Even if DFPS is not required to provide notice to a parent of a child in the managing conservatorship of DFPS as provided by Tex. Fam. Code § 264.018(h), DFPS shall provide notice under Tex. Fam. Code § 264.018 to a parent's attorney if the parent is represented by an attorney if:
• DFPS cannot locate the parent; or
• The child is in the PMC of DFPS and the parent has not participated in the child's case for at least six months despite DFPS' efforts to involve the parent. Tex. Fam. Code § 264.018(h-1).
A person entitled to notice from DFPS under Tex. Fam. Code § 264.018 must provide current contact information pursuant to Tex. Fam. Code § 264.018(j).
D. Judicial Review
The judiciary is charged with oversight of the safety, permanency, and well-being of the children in their courts. Tex. Fam. Code § 266.007 requires that the judge overseeing the case review a summary of the medical care being provided to the child at each hearing held pursuant to Tex. Fam. Code Chapter 263, specifically the Permanency Hearings Before and After Final Order.
1. Court Shall Review Medical Summary
Tex. Fam. Code Chapter 266 requires the summary of medical care to include:
• The nature of any emergency medical care provided to the child and the circumstances necessitating emergency medical care, including any injury or acute illness suffered by the child;
• All medical and mental health treatment that the child is receiving and the child's progress with the treatments;
• Any medication prescribed for the child and the condition, diagnosis, and symptoms for which the medication was prescribed and the child's progress with the medication;
• The degree to which the child or foster care provider has complied or failed to comply with any plan of medical treatment for the child;
• Any adverse reaction to or side effects of any medical treatment provided to the child;
• Any specific medical condition of the child that has been diagnosed or for which tests are being conducted to make a diagnosis; and
• Any activity that the child should avoid or should engage in that might affect the effectiveness of the treatment, including physical activities, other medications, and diet. Tex. Fam. Code § 266.007.
Additional information may be required to effectively oversee that informed consent has been given. Tex. Fam. Code Chapter 266 requires that judges review the medical care at each hearing conducted under Tex. Fam. Code Chapter 263.
The court must determine whether the child has been provided the opportunity, in a developmentally appropriate manner, to express opinion about medical care. Tex. Fam. Code § 263.306(a-1)(5)(D). For a child receiving psychotropic medication, the court must determine whether the child has:
• Been provided appropriate psychosocial therapies, behavior strategies, and non-pharmacological interventions; and
• Seen their prescribing physician at least every 90 days for review. Tex. Fam. Code § 263.306(a-1)(5)(F).
2. Youth in Foster Care Must Be Heard at Each Hearing Held Under Tex. Fam. Code Chapter 263
The Family Code provides that sixteen and seventeen-year-olds can serve as their own medical consenter with a judicial determination that the youth is capable of the role. Tex. Fam. Code § 266.010. If the youth is not the medical consenter, Tex. Fam. Code § 266.007(c) requires that the youth be provided the opportunity to express to the court their views on the medical care being provided. Further, Tex. Fam. Code § 263.302 requires that the youth attend Permanency Hearings Before and After Final Order.
Special Issue: Although it may be difficult to routinely include youth in their hearings, supporting youth attendance and participation in hearings is very important. This is especially impactful for older youth, as they are more likely than younger youth to be prescribed psychotropic medications.
The regular use of videoconferencing has now made it easier for youth to attend hearings and judges should consider the mental health benefits of doing so for a youth when given the opportunity for youth to advocate for themselves. For more ideas on involving youth in the court process, see the Child and Youth Voice chapter of this Bench Book.
3. Judicial Psychotropic Medication Information Line
Judges can contact the Judicial Medication Information Email Box which allows judges to submit a request for general medication information to SH_JudicialMailbox@superiorhealthplan.com. Judges should expect a response to general questions within 5 business days. Additionally, Superior HealthPlan now has a Manager of Service Coordination dedicated to their judicial program. Veronica Perkins can be reached at Veronica.A.Perkins@superiorhealthplan.com or by cell at 210-262-2769.
Emails are reviewed by a STAR Health Behavioral Health Service Coordinator, who has support from the STAR Health Behavioral Health Team, including a Medical Director (child psychiatrist), a Clinical Pharmacist, and Clinical Managers. (An example of an appropriate type of question for the email box is: “What are the side effects of a medication or combination of medications on a 12-year-old girl who weighs 100 pounds?”)
The STAR Health MCO also maintains a 24/7 Behavioral Health hotline with access to behavioral health professionals when urgent needs arise. The hotline can be reached at 1-866-912-6283. For more details on this program, see Health Care for Texas Children in Foster Care: STAR Health chapter of this Bench Book.
4. Some Courts Use Standardized Court Report
A standardized court report may help provide a summary of medical information that directly follows Tex. Fam. Code § 266.007. A standardized report may include the child's age and weight as well as information about medication and dosage, condition and diagnosis, symptom(s) being treated, last medication review, and the prescribing physician.
5. Some Courts Use Specific Forms and Practices
Some Texas child welfare judges have adopted a practice of ordering that in non-urgent situations, medical consenters must appear in court before giving consent to medication treatments that fall outside the Parameters. Also, to augment the information-sharing process, some judges ask the medical consenters to complete a checklist of questions before appearing in court to ensure that the consenter considered the many steps to informed consent (as defined by the Parameters).
Substance Use Disorders
A. Statewide Overview of Substance Use
The impact of a Substance Use Disorder (SUD) on the family and individual family members merits attention, as each family and each family member is uniquely affected by the person using substances. Impacts of substance use on the family may include financial challenges, legal problems, and emotional distress.[151]According to the National Center on Substance Abuse and Child Welfare parental substance use was a condition associated with removal in 76.7% of children under the age of one and 62.6% of children over the age of one in Texas in 2021.[152]
1. Relevant Trends
According to the Department of State Health Services, in 2023 there were over 4,900 deaths due to Unintentional Drug Poisoning in Texas.[153] Additionally, data from the 2023 Treatment Episode Data Set showed the top six primary substances among admissions to treatment services in Texas included Alcohol, followed by Methamphetamines, Heroin, Other Opiates/Synthetics, Marijuana/Hashish, and Cocaine.[154] Texas Health and Human Services Commission (HHSC) funds an array of substance use services to help individuals and families address substance use and misuse. For more information, please visit HHSC Substance Use Disorder Services webpage.
For information about drug-related deaths and trends in Texas, please visit the Department of State Health Services Texas Health Data Dashboard.[155]
2. Useful Definitions:
• Substance Use: The use—even one time—of any substance.[156]
• Substance Misuse: The use of any substance in a manner, situation, amount, or frequency that can cause harm to users or to those around them. For some substances or individuals, any use would constitute misuse (e.g., under-age drinking, injection drug use).[157]
• Substance Use Disorder (SUD): A medical illness caused by repeated misuse of a substance or substances. According to the DSM-5, substance use disorders are characterized by clinically significant impairments in health, social function, and impaired control over substance use and are diagnosed through assessing cognitive, behavioral, and psychological symptoms.[158]
• Recovery: a process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential. The process of recovery is highly personal and occurs via many pathways. It may include clinical treatment, medications, faith-based approaches, peer support, family support, self-care, and other approaches. Recovery is characterized by continual growth and improvement in one's health and wellness and managing setbacks. Because setbacks are a natural part of substance use, resilience becomes a key component of recovery.[159]
Every public health region in Texas has an Outreach, Screening, Assessment and Referral (OSAR) program which can assist any Texas resident with finding appropriate treatment and community resources. To find local resources and additional assistance, please visit the HHSC OSAR webpage.[160] Individuals can also locate substance use services in their area by visiting the Health and Human Services - Substance Use Service Locations map.[161]
B. Pregnant Women and Relapse Prevention and Safety Plans
1. Pregnant Women and Substance Use
Neonatal abstinence syndrome (NAS) is a treatable condition that newborns may experience as a result of prenatal exposure to certain substances, most often opioids. Neonatal Opioid Withdrawal Syndrome (NOWS) is a related term that refers to the symptoms that infants may experience as a result of exposure to opioids.[162] Pregnant women using opioids should not discontinue opioid use due to the risk of maternal return to use, overdose, withdrawals, and fetal demise. The American College of Obstetricians and Gynecologists (ACOG) and SAMHSA recommend Medications for Opioid Use Disorder (MOUD), previously referred to as Medication Assisted Treatment or MAT, as a best practice in managing an opioid use disorder in pregnancy.[163] Research also indicates women with substance use disorder should continue their opioid agonist pharmacotherapy (MOUD) postpartum. The postpartum period represents a time of increased vulnerabilities, and women with opioid use disorder experience recurrence far more often in the postpartum period compared with during pregnancy.[164]
Since 1994, SAMHSA has designated pregnant women as a federal priority population in SUD treatment services. To better meet the needs of this priority population HHSC has a variety of substance use treatment services specifically designed to treat pregnant women and women with dependent children including withdrawal management, residential and outpatient treatment, and Medications for Opioid Use Disorder.
Special Issue: “Medication for Opioid Use Disorder” (MOUD) is the recommended term to replace MAT. “Return to use” is the recommended term to avoid shame and stigma associated with the term “relapse,” however “relapse” and “relapse prevention” are still commonly used terms.
2. Recurrence/Return to Use Prevention
According to the National Center on Substance Abuse and Child Welfare, research shows medications used in MOUD, when provided at the proper dose, have no adverse effects on a person's intelligence, mental capability, physical functioning, or employability. Medications for Opioid Use Disorder, along with a range of clinical and supportive services, can help people achieve stability while focusing on other aspects of their recovery, such as finding work, housing, or enhancing their parenting skills.[165]
At this time, there are no standardized resources statewide for the Department of Family and Protective Services (DFPS). Department of Family and Protective Services accesses state-funded and community resources that offer individualized treatment approaches to meet the needs of parents and families. Relevant DFPS policy states the following regarding recurrence (relapse) prevention planning:
• Relapse is a return to a pattern of substance use after a period of non-use.
• In the relapse safety plan, the person, along with a trusted support system, plans to ensure the safety of the child or children in case relapse becomes an issue.
• Court orders supersede any actions that the person requests in the relapse safety plan.
• A relapse safety plan can be developed at any stage of service.”
Please see Developing a Safety Plan in Case a Client Relapses CPS Policy Handbook § 1982.2 for more information.[166]
C. DFPS Response to Substance Use Disorders
The Child Abuse Prevention and Treatment Act (CAPTA) (P.L. 93-247) was originally enacted in 1974, was last reauthorized in 2010, and amended most recently in 2019; additionally, certain provisions were amended by the Comprehensive Addiction and Recovery Act (CARA) of 2016 and the Victims of Child Abuse Act Reauthorization Act of 2018 (P.L. 115-424).[167]
Under these federal laws, states are required to have plans of safe care for infants born and identified as being affected by substance use or withdrawal symptoms of both legal and illegal substances. The plans of safe care are required to “ensure the safety and well-being of such infant following [the infant's] release from the care of healthcare providers” to be achieved through “addressing the health and substance use disorder treatment needs of the infant and affected family or caregiver.” 42 U.S.C.S. § 5106a(b)(1)-(2).
To avoid confusion, DFPS does not utilize the unique federal term “plan of safe care” as set forth in CARA, as there are a number of DFPS tools and policies that reference “plans.” Statewide Intake protocols, safety and risk assessment tools, and the service planning process used in different stages of service, collectively mean that the state meets the requirements under the CARA plans of safe care.
Examples of types of plans that do not include removal include: use of Parental Child Safety Placements (PCSP) to assure safety as the parent initiates or becomes engaged in services; use of residential substance use disorder treatment programs that allow a mother (or father in a few programs) to live in a treatment setting with the child, when appropriate; use of Medication-Assisted Treatment in combination with behavioral therapies; and the guidance of specialized drug courts in some areas. While access to treatment can be challenging, families referred by DFPS are considered a state priority population for state-funded substance use intervention and treatment services. In Texas, a client who is not pregnant and is referred to an HHSC-funded substance use intervention or treatment service by DFPS must be admitted to services within 72 hours or 3 business days, depending on the program or services.
Doctors and nurses are required by mandatory reporting laws to report suspected child abuse and neglect if they have reasonable cause to believe the child has been abused as defined by statute. Tex. Fam. Code § 261.101(b). Definitions of child abuse in Texas law include the current use of controlled substances by an adult in a manner or to the extent that the use results in physical, mental, or emotional injury to a child. Tex. Fam. Code § 261.001(1)(I).
DFPS Statewide Intake advances any reports of substance-exposed infants to the field for an investigation. During the investigation, multiple steps occur including: a child assessment, parental assessment, holistic family assessment, safety planning, and the development of initial services. In some cases, the parent has sufficient support and is protective and/or engaged in treatment services, thereby eliminating the need for further DFPS involvement beyond investigation. Other parents may be assisted in development of a plan and access to services during the investigation stage of services, or a Family-Based Safety Services (FBSS) stage may be opened to provide ongoing services without removal. Where safety cannot be assured, DFPS will seek removal of the infant.
Special Issue: The birth of a substance-exposed infant does not result in an automatic removal of that child, nor even an automatic disposition of child abuse or neglect. Each family's specific circumstance is assessed. DFPS works closely with Health and Human Services agency partners who provide substance use intervention or treatment services to strengthen the State's response to parents who engage in substance use or misuse.
1. Behavioral Health Division at DFPS
DFPS has a Behavioral Health Services Division within CPS, with Behavioral Health and Substance Use Disorder Specialists spread throughout the state. The division is part of a broader CPS Medical Services Division that supports staff meeting medical, behavioral health, and dental needs for children in DFPS conservatorship. The Behavioral Health Division also provides support and subject matter expertise to staff in Family-Based Safety Services, where children are not in DFPS conservatorship. The combined Medical and Behavioral Health teams assist legacy and SSCC direct delivery staff with access to Medicaid services (STAR Health) and other public behavioral health services available to children and families. The broader team includes Well-Being Specialists, Nurse Consultants, CANS Program Specialist, and supporting staff. These positions complement two additional Substance Use Program Specialists and two Mental Health Program Specialists who report to Child Protective Investigations. The combined team works together to overcome barriers to services, and provide support, resources, and technical assistance to direct delivery staff in their work with families and youth through every stage of service.
D. Resources
• American Addiction Centers' Information on Addiction Signs, Symptoms, Effects, and Treatment[168] and Addiction Cravings: Symptoms, Treatment and Relapse Prevention[169]
• Children and Family Futures[170]
• Child Welfare Information Gateway Information on Family Treatment Drug Court[171]
• National Center on Substance Abuse and Child Welfare (NCSACW)[172]
• National Council of Juvenile and Family Court Judges Substance Use and the Courts (NCJFCJ)[173]
• National Institute on Drug Abuse[174]
• Substance Abuse and Mental Health Services Administration (SAMHSA)[175]
• Texas Health and Human Services Mental Health and Substance Use
Trauma-Informed Care
Introduction
A. Trauma
The concept of trauma and the accompanying research have shifted the paradigm about the way in which systems, organizations, professionals, and caregivers approach and serve children, youth, young adults, parents, and families who experience the child welfare system. The field of trauma and trauma-informed care is constantly evolving and expanding. The information in this chapter is intended to give judges a basic understanding of these topics to help them consider approaching child welfare cases in a trauma-informed manner.
40 Tex. Admin. Code § 702.701(a) defines trauma as resulting from "an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening with lasting adverse effects on the individual's functioning or the individual's mental, physical, social, emotional, or spiritual well-being."[176]
Some examples of traumatic experiences include:[177]
• Physical, sexual, or psychological abuse and neglect (including trafficking);
• Witnessing and/or experiencing violence, whether in the family or in the community;
• Loss of loved ones or traumatic grief;
• Natural and technological disasters or terrorism;
• Serious accidents;
• Medical trauma; and/or
• Military family-related stressors (e.g., deployment, parental loss, or injury)
B. Trauma Impacts a Child's Development and Health
The groundbreaking 1998 study on Adverse Childhood Experiences (ACEs) and the replicated studies which followed demonstrate that a high number of ACEs and the related experience of childhood stress is linked to poor health outcomes, including obesity, diabetes, depression, heart disease, cancer, and stroke as well as alcohol and drug abuse, low graduation rates, and poor employment outcomes.[178] The presence of ACEs does not mean that a child is guaranteed to experience poor life outcomes. Positive experiences and protective factors can prevent children from experiencing adversity and protect against many negative health and life outcomes.[179]
Undoubtedly, children and youth who experience abuse or neglect, are removed from their families, or interact with the child welfare system are vulnerable to experiencing trauma. Further, many parents and caregivers may have their own experiences with trauma. Families experiencing the child welfare system are more likely to feel supported and build resilience if the child welfare system and adjacent systems can respond to the needs of children and families through a trauma-informed lens. This requires judges, attorneys, court staff, and other stakeholders to understand how traumatic responses manifest in the children and families in front of the court and subsequently consider adapting the court environment and practices accordingly. In doing so, serving children and families can move beyond responding to behaviors to promoting healing.
It is important to note that no age is immune to the effects of traumatic experiences, including infants and toddlers. Traumatic stress will manifest differently from child to child and will depend on the child's age and developmental level.[180]
Children who are not experiencing consistent safety, comfort, and protection may develop ways of coping that allow them to survive and function day-to-day. These learned adaptations make sense when a physical and/or emotional threat is pervasive but are not helpful once a person is no longer under such threats.[181] Additionally, unaddressed trauma can lead to long-term effects into adulthood.
Some potential effects of trauma are:[182]
• Difficulties with emotional regulation, focus, and self-control (when in fight or flight mode, the brain loses executive functions that do not serve fight or flight, such as higher learning and problem-solving which contribute substantially to school success);
• Anxious and/or avoidant behaviors;
• Difficulty developing strong, healthy attachment to caregivers and others;
• Distrust of people in authority, who may be seen as threats;
• Over-responding or under-responding to sensory stimuli;
• Misinterpreting motives, facial expressions, and/or body language in others;
• Feeling isolated and/or having difficulty playing well with others;
• Difficulty with problem solving and/or decision-making;
• Chronic or recurrent physical complaints;
• Potential impacts to self-efficacy; and/or
• More likely to engage in high-risk behaviors.
C. Trauma-Informed Child Welfare System
40 Tex. Admin. Code § 702.701(b) defines trauma-informed as:
An individual, program, organization, or system that is trauma-informed fully integrates knowledge about trauma into policies, procedures, and practices by:
• Realizing the widespread impact of trauma, understanding potential paths for recovery, and acknowledging the compounding impact of structural inequities related to culture, history, race, gender, identity, locale, and language;
• Recognizing the signs and symptoms of trauma in clients, families, staff, and others involved with the system;
• Maximizing physical and psychological safety and responding to the impact of structural inequities on individuals and communities;
• Building healthy, trusting relationships that create mutuality among children, families, caregivers, and professionals at an individual and organizational level; and
• Striving to avoid re-traumatization.
D. Statutory Requirements for Trauma-Informed Care Training
1. Training for Attorney Ad Litems
As of September 1, 2021, an attorney who is on the list maintained by the court as being qualified for appointment as an attorney ad litem for a child in a child welfare case must provide proof that the attorney has completed a training program regarding trauma-informed care and the effect of trauma on children in DFPS conservatorship. Attorneys should complete the training as soon as practicable once placed on the appointment list. Thereafter, an attorney must provide proof each year of compliance with the statute. Tex. Fam. Code § 107.004(b)-(b-3).
An attorney ad litem is responsible for periodically reviewing the child client's safety and well-being, including effects of trauma to the child. Tex. Fam. Code § 107.004 (d-3). Attorney ad litem training must include information regarding:
• The symptoms of trauma and the impact that trauma has on a child, including how trauma may affect a child's development, emotions, memories, behavior, and decision-making;
• Attachment and how a lack of attachment may affect a child;
• The role that trauma-informed care and services can have in a child's ability to build connections, feel safe, and regulate the child's emotions to help the child build resiliency and overcome the effects of trauma and adverse childhood experiences;
• The importance of screening children for trauma and the risk of mislabeling and inappropriate treatment of children without proper screening, including the risks and benefits associated with the use of psychotropic medication;
• The potential for re-traumatization of children in DFPS Conservatorship; and
• The availability of:
◦ research-supported, trauma-informed, non-pharmacological interventions; and
◦ trauma-informed advocacy to increase a child's access, while the child is in DFPS conservatorship, to:
▪ trauma-informed care; and
▪ trauma-informed mental and behavioral health services. Tex. Fam. Code § 107.004(b-4).
2. DFPS Training
In 2011, the Texas Family Code was amended to require DFPS to include training in trauma-informed programs and services in any training which DFPS provides to foster parents, adoptive parents, kinship caregivers, department caseworkers, and department supervisors. Tex. Fam. Code § 264.015.
DFPS caseworkers are required to complete an initial, in-person training on trauma-informed care during their basic skills development training and an annual refresher course online. Supervisors and mentors are also required to complete a secondary trauma training. DFPS internal learning management system offers several optional trainings on trauma-related topics.
3. Residential Child Care Contract (RCCC) Requirements
As of September 1, 2015, DFPS required all caregivers and employees who are subject to RCCC for direct care to complete:
• At least eight hours of trauma-informed care training prior to being the only caregiver responsible for children; and
• At least two hours of trauma-informed care annually, and contractors may select their own curriculum/model for the annual refresher training.[183]
Since 2015, DFPS and SSCC organizations are required to institute a comprehensive psychosocial assessment tool to assess all children who enter the foster care system within 45 days. The tool must include a trauma assessment and an interview with at least one individual who knows the child. DFPS utilizes the Child and Adolescent Needs and Strengths (CANS) to assess children and youth placed in substitute care ages 3 to 17 years within 30 days. Tex. Fam. Code § 266.012.
4. Related Fields
Since 2013, the Texas Human Resources Code requires trauma-informed care training for certain staff of county and state juvenile facilities, including probation officers, supervision officers, correctional officers, parole officers and court-supervised community-based program personnel. Tex. Hum. Res. Code § 221.002(c-1) and Tex. Hum. Res. Code § 221.0061.
E. Emergency Behavior Interventions
Many trauma-informed care trainings promote specific strategies including self-care approaches, peer-provided services, arts programs, and comfort rooms to enhance healing and to provide a means to avoid the use of restraint and seclusion. Generally, if a trauma response is triggered, allowing time, space, and support can help re-establish self-regulation.
In Texas, the Administrative Code offers the following guidelines on utilizing Emergency Behavior Interventions, such as restraints and seclusion, on children in General Residential Operations and Residential Treatment Centers. These guidelines are summarized in the chart which follows.
1. Restraint/Seclusion May Only Be Used:
• As last resort
26 Tex. Admin. Code § 748.2455(a)(1) and (2); 26 Tex. Admin. Code § 749.2055(a)(1) and (2); 26 Tex. Admin. Code § 748.2551(a); and 26 Tex. Admin. Code § 749.2151
• After less restrictive and more positive measures have been tried and failed
26 Tex. Admin. Code § 748.2455(a)(1) and (2); 26 Tex. Admin. Code § 749.2055(a)(1) and (2); 26 Tex. Admin. Code § 748.2551(a); and 26 Tex. Admin. Code § 749.2151(a)
• Only in an emergency situation or to administer intra-muscular medication or other physician prescribed medication
26 Tex. Admin. Code § 748.2455(a)(2); 26 Tex. Admin. Code § 749.2055(a)(2); 26 Tex. Admin Code § 748.43(22); and 26 Tex. Admin. Code § 749.43(25) (Definition of emergency situation)
• When immediately necessary
26 Tex. Admin. Code § 748.43(20); 26 Tex. Admin. Code § 749.43(23) (Definition of Emergency Behavioral Intervention (EBI); 26 Tex. Admin Code § 748.43(22); and 26 Tex. Admin. Code § 749.43(25) (Definition of emergency situation)
• To prevent imminent probable death or substantial physical injury
26 Tex. Admin. Code § 748.43(20); 26 Tex. Admin. Code § 749.43(23) (Definition of EBI); 26 Tex. Admin. Code § 748.43(22); 40 Tex. Admin. Code § 749.43(25) (Definition of emergency situation); 26 Tex. Admin. Code § 748.43(68); and 26 Tex. Admin. Code § 749.43(72) (Definition of substantial physical injury)
• Never as punishment, retaliation, means of compliance, convenience, or treatment
26 Tex. Admin. Code § 748.2463 and 26 Tex. Admin. Code § 749.2063
2. Types of Restraints That May Be Administered with Restrictions:
• Short personal restraint and personal restraint
26 Tex. Admin. Code § 748.2451(a)(1) and (2); 26 Tex. Admin. Code § 749.2051(a)(1) and (2); 26 Tex. Admin. Code § 748.43(51) and (65); and 26 Tex. Admin. Code § 749.43(52) and (69) (Definition of personal restraint and short personal restraint)
• Emergency medication
26 Tex. Admin. Code § 748.2451(a)(3); 26 Tex. Admin. Code § 749.2051(a)(3); 26 Tex. Admin. Code § 748.2753 (simultaneous use with another EBI); 26 Tex. Admin. Code § 749.2233 (simultaneous use with personal restraint); 26 Tex. Admin. Code § 748.43(21); and 26 Tex. Admin. Code § 749.43(24) (Definition of emergency medication)
• Seclusion
26 Tex. Admin. Code § 748.2451(a)(4); 26 Tex. Admin. Code § 748.2651; 26 Tex. Admin. Code § 748.43(63); 26 Tex. Admin. Code § 749.43(67) (Definition of seclusion); and 26 Tex. Admin. Code § 749.2051(b)
• Mechanical restraint
26 Tex. Admin. Code § 748.2451(a)(5) (only in Residential Treatment Centers); 26 Tex. Admin. Code § 748.2701; 26 Tex. Admin. Code § 748.2703; 26 Tex. Admin. Code § 748.2755 (simultaneous use with emergency medication); 26 Tex. Admin. Code § 748.43(39); 26 Tex. Admin. Code § 749.43(40) (Definition of mechanical restraint); and 26 Tex. Admin. Code § 749.2051(b)
3. Restraint/Seclusion May Only Be Administered by:
• A caregiver qualified in emergency behavior interventions
26 Tex. Admin. Code § 748.2453; 26 Tex. Admin. Code § 749.2053; (Requirements); 26 Tex. Admin. Code § 748.947; 26 Tex. Admin. Code § 749.947 (Annual training requirements)26 Tex. Admin. Code § 748.863(a); 26 Tex. Admin. Code § 749.863(a) (Pre-service training requirements); 26 Tex. Admin. Code § 748.930; and 26 Tex. Admin. Code § 749.930 (Training hours).
• Whose duties include the direct care, supervision, guidance, and protection of child
• 26 Tex. Admin. Code § 748.43(5) and 26 Tex. Admin. Code § 749.43(9)
Figure: 26 Tex. Admin. Code § 748.2553
|
Type of Emergency Behavior Intervention |
The caregiver must release the child if any of the following apply: |
|
(1) Short personal restraint |
(A) Immediately when an emergency health situation occurs during the restraint and the caregiver must obtain treatment immediately; or (B) Within one minute, or sooner if the danger is over or the emergency situation no longer exists. |
|
(2) Personal restraint |
(A) Immediately when an emergency health situation occurs during the restraint. The caregiver must obtain treatment [for the child] immediately; (B) Within one minute of the implementation of a prone or supine transitional hold; (C) As soon as the child's behavior is no longer a danger to himself or others; (D) As soon as the medication is administered; or (E) When the maximum time allowed for personal restraint is reached. |
|
(3) Emergency medication |
Not applicable. |
|
(4) Seclusion |
(A) Immediately when an emergency health situation occurs during the seclusion and the caregiver must obtain treatment immediately; (B) As soon as the child's behavior is no longer a danger to himself or others; (C) No later than five minutes after the child begins exhibiting the regulated behaviors[184]; (D) When the maximum time allowed for seclusion is reached; (E) If the child falls asleep in seclusion, the caregiver must: (i) Unlock the door; (ii) Continuously observe the child until he awakens; and (iii) Evaluate his overall well-being; or (F) If the child is receiving emergency care services: (i) As soon as the child is no longer a danger to himself or others; (ii) Upon the arrival of a medical professional; or (iii) Upon assistance from law enforcement or the fire department. |
|
(5) Mechanical restraint |
(A) Immediately when an emergency health situation occurs during the restraint and the caregiver must obtain treatment immediately; (B) As soon as the child's behavior is no longer a danger to himself or others; (C) No later than five minutes after the child begins exhibiting the regulated behaviors; (D) When the maximum time allowed for mechanical restraint is reached; or (E) If the child falls asleep in the mechanical restraint. In this situation, the caregiver must release the child from the restraint and continuously observe the child until he awakens and evaluate him. |
4. A Child Must Be Released from a Restraint/Seclusion:
• Immediately if an emergency health situation arises
26 Tex. Admin. Code § 748.2553(1)(A), (2)(A), (4)(A), and (5)(A); 26 Tex. Admin. Code § 749.2153(1)(A) and (2)(A); 26 Tex. Admin. Code § 748.2603; and 26 Tex. Admin. Code § 749.2203
• Immediately once the danger is over
26 Tex. Admin. Code § 748.2553(2)(C) and 26 Tex. Admin. Code § 749.2153(2)(C)
• Once maximum time allowed is reached
26 Tex. Admin. Code § 748.2553(2)(E); 26 Tex. Admin. Code § 749.2153(2)(E); and 26 Tex. Admin. Code § 748.2553(2)(E) and (4)(D)
Figure: 26 Tex. Admin. Code § 748.2801
|
Types of Emergency Behavior Intervention |
The maximum length of time is: |
|
(1) Short personal restraint |
One minute. |
|
(2) Personal restraint |
(A) For a child of any age, 30 minutes; (B) A prone or supine personal restraint transitional hold may not exceed one minute. |
|
(3) Emergency medication |
Not applicable. |
|
(4) Seclusion |
(A) For a child under nine years old, one hour. (B) For a child nine years old or older, two hours. |
|
(5) Mechanical restraint |
(A) For a child under nine years old, 30 minutes. (B) For a child nine years old or older, one hour. |
When restraining/secluding, a written order is required:
• By a licensed physician when administering emergency medications
26 Tex. Admin. Code § 748.2501(3) and 26 Tex. Admin. Code § 749.2101(3)
• By a licensed psychiatrist when administering mechanical restraints
26 Tex. Admin. Code § 748.2501(5)
• By a licensed psychiatrist, physician, or psychologist when administering successive restraints
26 Tex. Admin. Code § 748.2501(2); 26 Tex. Admin. Code § 749.2101(2)(A); 26 Tex. Admin. Code § 748.2751(3); and 26 Tex. Admin. Code § 749.2231(a)
• When using restraints simultaneously
26 Tex. Admin. Code § 748.2501(2); 26 Tex. Admin. Code § 749.2101(2)(A); 26 Tex. Admin. Code § 748.2753(a)(3) and (b); 26 Tex. Admin. Code § 749.2233(a) (Emergency medications with personal restraint); and 26 Tex. Admin. Code § 748.2755(a)(3) and (b) (Mechanical restraints with emergency medications)
• When maximum length of time allowed is exceeded
26 Tex. Admin. Code § 748.2805; however under 26 Tex. Admin. Code § 749.2283, time extension prohibited.
• Also see: 26 Tex. Admin. Code § 748.2505; 26 Tex. Admin. Code § 749.2105 (Content of written orders); 26 Tex. Admin. Code § 748.2507; 26 Tex. Admin. Code § 749.2107 (PRN orders); and 26 Tex. Admin. Code § 748.2807 (verbal orders to exceed maximum time allowed)
Figure: 26 Tex. Admin. Code § 748.2501
|
Type of Emergency Behavior Intervention |
Are written orders required to administer the intervention for a specific child? |
Who can write orders for the use of the intervention for a specific child? |
|
(1) Short personal restraint |
NO. |
Not applicable. |
|
(2) Personal restraint |
NO. However, successive restraints, a restraint simultaneous with emergency medication, and/or a restraint that exceeds the maximum time limit all require orders as specified in this subchapter. PRN orders are also permitted under 26 Tex. Admin. Code § 748.2507 of this title (relating to “Under what conditions are PRN orders permitted for a specific child?”). |
Not applicable. |
|
(3) Emergency medication |
YES. |
A licensed physician. |
|
(4) Seclusion |
YES, except written orders are not required when [professionals] provide emergency care services to the child placed in seclusion. |
A licensed psychiatrist, psychologist, or physician. |
|
(5) Mechanical restraint |
YES. |
A licensed psychiatrist. |
A review of the use of emergency behavior intervention for a specific child is triggered when:
• Personally restrained four times in a seven-day period or more than 12 times in 30-day period or same child personally restrained more often than order allows.
26 Tex. Admin. Code § 748.2901(a)(2) and 26 Tex. Admin. Code § 749.2331(b)(2)
• Emergency medications used three times in a thirty-day period
26 Tex. Admin. Code § 748.2901(3) and 26 Tex. Admin. Code § 749.2331(3)
• Secluded more than twelve hours or three times in a seven-day period
26 Tex. Admin. Code § 748.2901(a)(4) (Note that this is not applicable to foster care placements.)
• Mechanically restrained more than three hours or three times in a seven-day period
26 Tex. Admin. Code § 748.2901(a)(5) (Note that this is not applicable to foster care placements.)
Restraint/Seclusion that is NOT allowed:
• Mechanical restraint may not be simultaneously used with seclusion or pursuant to PRN order
26 Tex. Admin. Code § 748.2757 and 26 Tex. Admin. Code § 748.2507(5)
• No chemical restraints
26 Tex. Admin. Code § 748.1119(1); 26 Tex. Admin. Code § 749.1021(1); 26 Tex. Admin. Code § 748.2451(b); 26 Tex. Admin. Code § 749.2051(b); 26 Tex. Admin. Code § 748.43(7); and 26 Tex. Admin. Code § 749.43(12) (Definition)
• Prone or supine restraints except for a transitional hold for 1 minute or less or as a last resort
26 Tex. Admin. Code § 748.2605(b); 26 Tex. Admin. Code § 749.2205(b) and (c); 26 Tex. Admin. Code § 748.2461(b)(1); 26 Tex. Admin. Code § 749.2061(b)(1); 26 Tex. Admin. Code § 748.2553(2)(B); 26 Tex. Admin. Code § 749.2153(2)(B); 26 Tex. Admin. Code § 748.2801(2)(B); and 26 Tex. Admin. Code § 749.2281(2)(B)
• Foster care placements may never administer chemical restraints, mechanical restraints, or seclusion.
Also see other relevant provisions:
• 26 Tex. Admin. Code § 748.1119 and 26 Tex. Admin. Code § 749.2051 (Techniques prohibited)
• 26 Tex. Admin. Code § 748.2303 and 26 Tex. Admin. Code § 749.1953 (May not use or threaten corporal punishment)
• 26 Tex. Admin. Code § 748.2307 and 26 Tex. Admin. Code § 749.1957 (Methods of punishment prohibited)
• 26 Tex. Admin. Code § 748.2605 and 26 Tex. Admin. Code § 749.2205 (Prohibited physical restraint techniques)
• 26 Tex. Admin. Code § 748.2705 (Types of mechanical & other restraint devices prohibited)
F. Trauma Work in Texas
1. Reports
Building a Trauma-Informed Child Welfare System: A Blueprint[185]
Trauma-Informed Care Final Report, The Meadows Mental Health Policy Institute for Texas[186]
Building a Network of Trauma Informed Courts in Texas, Texas Alliance of Child and Family Services [187]
2. Statewide Initiatives
a. The Statewide Collaborative on Trauma-Informed Care
In July 2017, the Children's Commission launched the Statewide Collaborative on Trauma-Informed Care (SCTIC), which aims to elevate trauma-informed policy in the Texas child welfare system by creating a statewide strategy to support system reform, organizational leadership, cross-systems collaboration, and community-led efforts with data-informed initiatives to develop champions, consensus, and funding. The SCTIC began with a planning group with the Children's Commission, Meadows Mental Health Policy Institute (MMHPI), Texas CASA, and the Department of Family and Protective Services and created workgroups to carry out its mission.
b. Behavioral Health Division at DFPS
In Fiscal Year 2019, DFPS formed the Behavioral Health Services Division within CPS, managed as a separate division within the CPS Medical Services Division. The division includes a Behavioral Health Services Division Administrator, three Behavioral Health Services Program Specialists, three Substance Use Program Specialists, one CANS Program Specialist, and a Mental Health Program Specialist Lead. The Medical Services Division is a statewide team that covers medical, physical, and dental issues for CPS with Nurse Consultants and Well-Being Specialists. The Medical Services Division focuses on the services provided through STAR Health. The Behavioral Health Services Division Administrator is located in Lubbock, Texas, and manages the statewide team which focuses on the public behavioral health system. The Behavioral Health Services Program Specialists are located in Houston, Fort Worth, and San Antonio, Texas. The Mental Health Program Specialist Lead is located in Waco, Texas. The CANS Program Specialist helps to manage the eCANS system, in which CANS 3.0 assessments for children in conservatorship are entered, and is located in Rockwall, Texas.
The division includes three Substance Use Program Specialists located in San Antonio, Dallas, and Houston, Texas. These positions complement two additional Substance Use Program Specialists and two Mental Health Program Specialists who report to Child Protective Investigations. These staff work together to provide support, resources, and technical assistance to direct delivery staff in their work with families experiencing substance use disorders through every stage of service.
Both the Medical Services and Behavioral Health Services teams not only support children in conservatorship, but also assist with investigations and Family-Based Safety Services cases when the need arises. Additionally, the teams work with CPS and SSCC staff statewide and are generally located in the regions they support.
In 2023, in accordance with Article II Rider 44 of the 88th Texas Legislature, the Department created the Office of Behavioral Health Strategy to provide coordination and cooperation between DFPS and the myriad of state funders and local providers of pediatric behavioral healthcare as a means to improve access to services for youth in DFPS conservatorship. The goals of the office are to identify the behavioral health needs of DFPS youth, address barriers to care, improve access to services, and identify and recommend ways to expand the capacity of the children's behavioral health system to meet the unique needs of youth in DFPS conservatorship. This includes recommendations on how to improve access to STAR Health services, address policy and procedural barriers, and improve behavioral health outcomes for DFPS involved children and youth.
c. Cross-Systems Trauma-Informed Care initiative
The Texas Health and Human Services Commission (HHSC) Office of Mental Health Coordination leads a Cross Systems Trauma-informed Care (CSTIC) initiative. The vision of the CSTIC is a coordinated behavioral health system, as envisioned by the Texas Statewide Behavioral Health Strategic Plan, which is healing-centered and trauma-informed in its foundation and unified in its implementation of a person-centered and family-focused approach across Texas. The CSTIC initiative involves working with state agencies across Texas to advance trauma-informed organizations, culture, and services. The collaboration includes representatives from state agencies who receive state funding for behavioral health training or services. As part of the CSTIC initiative, HHSC leads an internal Trauma Transformation Team with representatives from different divisions and departments within the agency who facilitate trauma-informed change within HHSC. Additionally, beginning in 2020, the Cross-Systems Trauma-Informed Care Projects Committee collaborated with The University of Texas at Austin Texas Institute for Excellence in Mental Health to develop free trauma-informed care training modules for professionals seeking high-quality, in-depth training. Over several years, the committee helped develop a multi-session, trauma-informed care training named Trauma-Informed Care Basics.
d. Children's Advocacy Centers (CAC) Practice Model
In 2013, the Texas Legislature raised the standard for mental health services in CACs, requiring that all mental health services be trauma-focused and evidence-based. Additionally, mental health services must be provided by professionals who have a master's degree and are licensed, or who are students in an accredited graduate program and supervised by a licensed mental health professional.
e. Trauma-Informed Care Specialty Network
Created by STAR Health, the Trauma-Informed Care Specialty Network allows its providers to list the training on trauma that they have pursued and helps identify providers who have been trained in trauma-informed care in the STAR Health network for caseworkers, caregivers, and others in the child welfare community. STAR Health also offers TIC trainings to CPA, kinship families, RTC staff, and Emergency Shelter staff.
3. Examples of Community-Level Initiatives
a. North Texas Foster Care Consortium
Established in 2015 to promote collaboration and information sharing among the many stakeholders committed to the well-being of children in the child welfare system. the North Texas Foster Care Consortium facilitates productive partnerships and sponsors informative programming, drawing on the resources of integrated healthcare and other service providers, child advocates, policy groups, child placing agencies, education liaisons, foster parents, court personnel, single source continuum contractors, and DFPS leadership.
b. The Travis County Collaborative for Children (TCCC)
Led by Texas Christian University's (TCU) Karyn Purvis Institute of Child Development (KPICD), the TCCC implemented system-wide changes to the way children in Travis County are cared for during and after their time in state custody. TCCC's goal is to accelerate healing and speed to permanency for children in foster care utilizing KPICD's research-based Trust-Based Relational Intervention (TBRI®) principles and practices.
c. The South Texas Trauma-Informed Care Consortium
The South Texas Trauma Informed Care Consortium is a collaboration between The Children's Shelter, Voices for Children, and City of San Antonio Metro Health Department that brings together community participants who are committed to addressing the impact of trauma.
G. National Resources
• NCJFCJ:
◦ Trauma-Informed Courtroom Practices: A Bench Card for Judges[188]
◦ Ten Things Every Juvenile Court Judge Should Know about Trauma and Delinquency[189]
◦ Assessing Trauma for Juvenile and Family Courts[190]
• National Center for State Courts Study of Virtual Child Welfare Hearings Facilitating Trauma-Responsive Virtual Hearings for Dependency Cases[191]
• National Child Traumatic Stress Network (NCTSN) Bench Cards for the Trauma-Informed Judge[192]
• Mental Health America (MHA) Position Statement on Seclusion and Restraint[193]
H. Training Resources
• Children's Commission's Judicial Trauma Institute[194]
• Trauma Informed Texas traumainformedtexas.com[195]
• DFPS Trauma-Informed Care Training[196]
• Superior HealthPlan, the STAR Health Managed Care Organization (MCO), offers online webinars through their parent organization, Centene Foster Care[198]